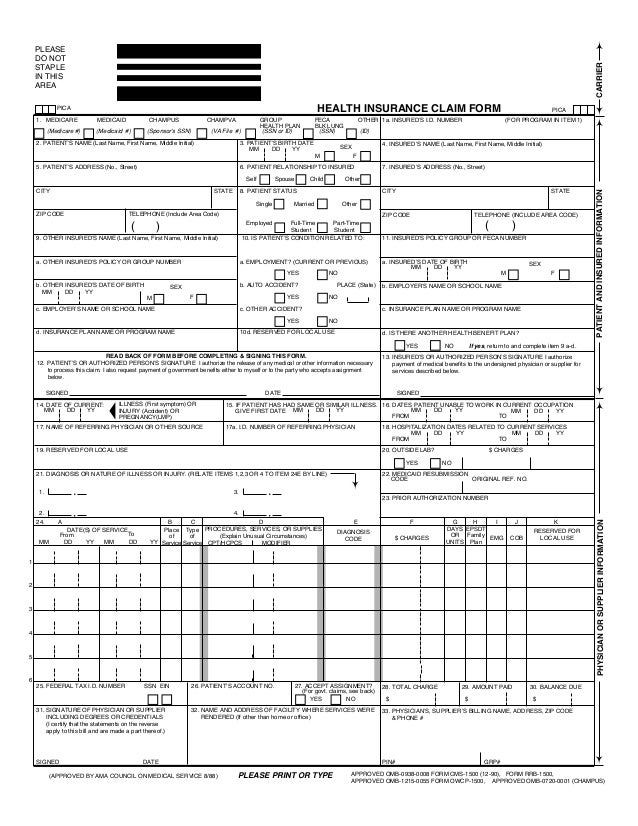
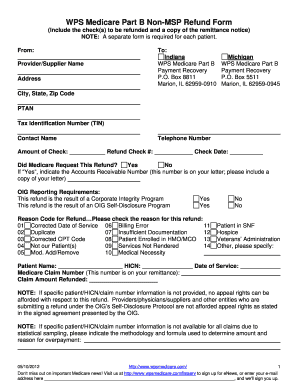
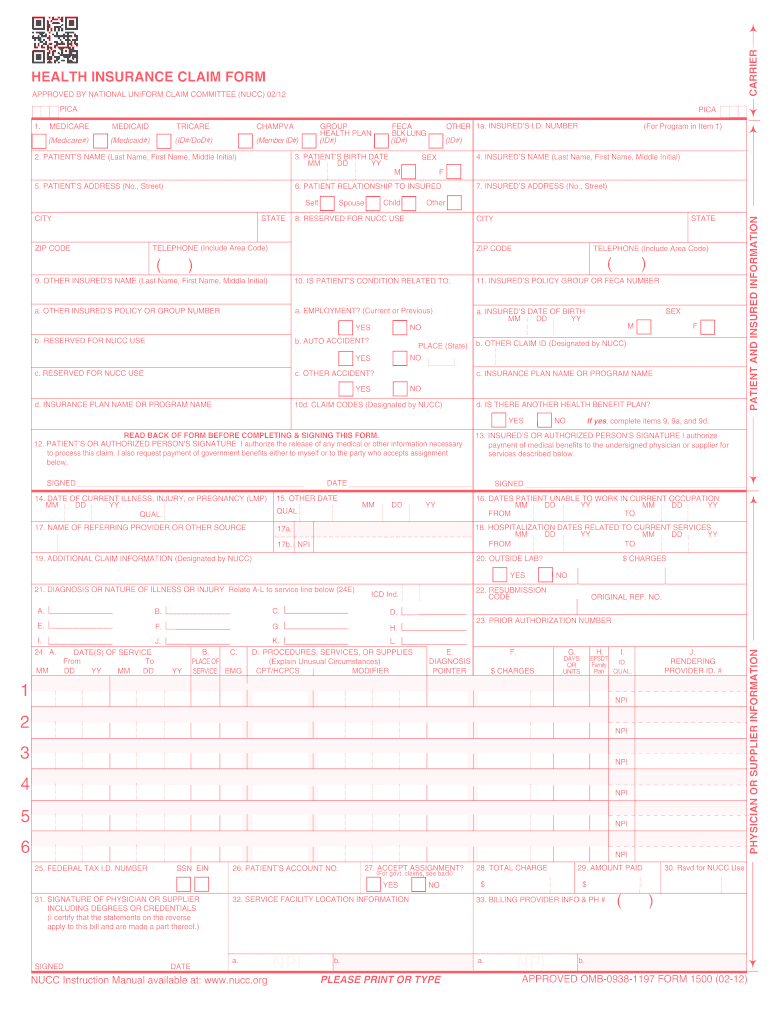
This part is easy. HEALTH INSURANCE CLAIM FORM.
![]() Forms And Resources Beacon Health Options
Forms And Resources Beacon Health Options
Yes No Yes No Please list.
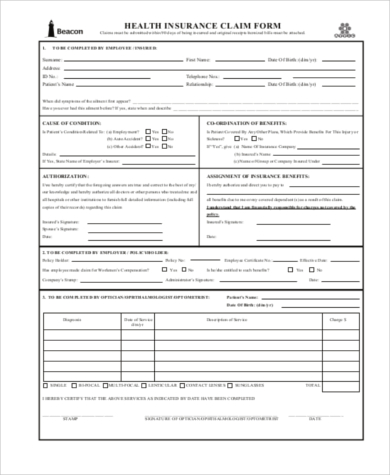
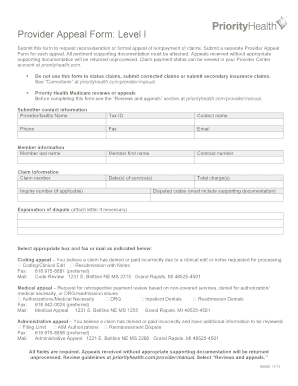
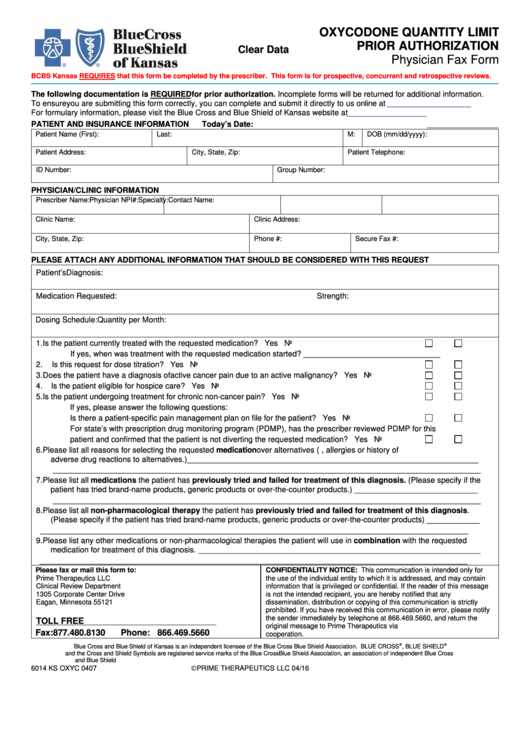
Beacon health claim form. Health care providers can submit this form for services provided to patients. Provider Form - Use this form to notify Beacon Health of the following. 2 months ago CMI Beacon Health Claim Form 0221f.
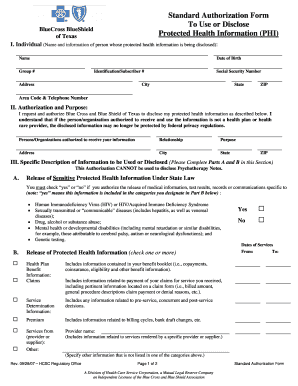
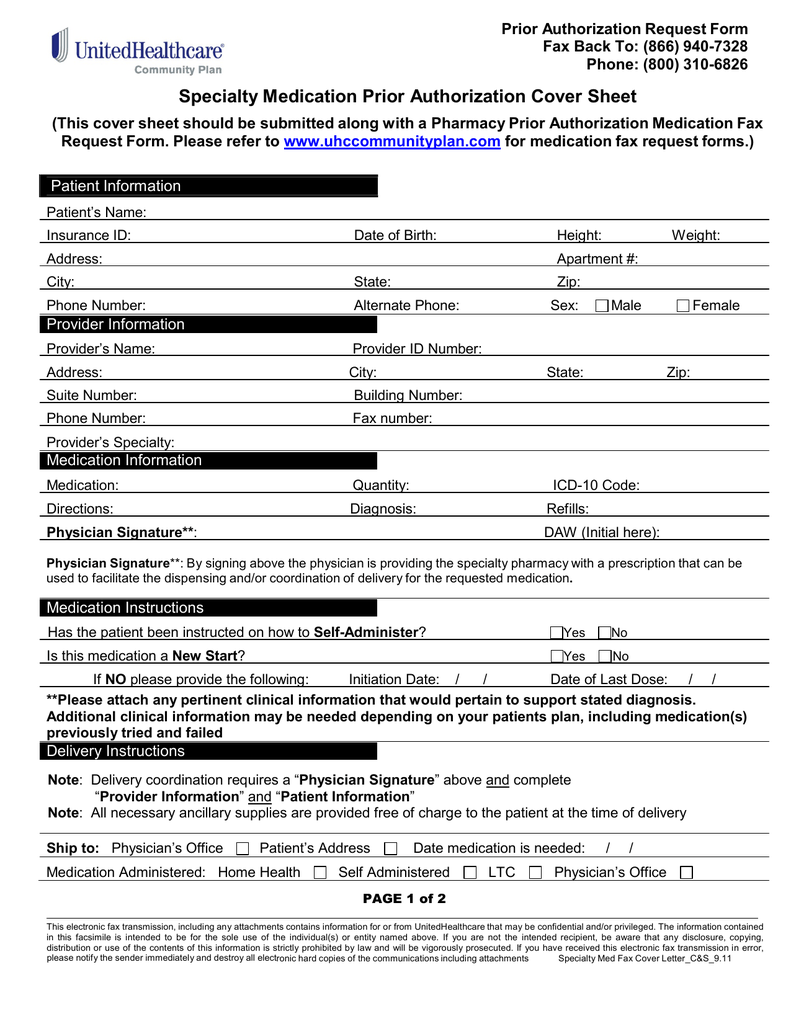
Authorization for Use or Disclosure of Medical Information. For all State Health Plan behavioral health telephone inquiries to Beacon Health Options call 800-367-6143. Also if a provider is unregistered they can self-register using the 6-digit Beacon Health Options ID.
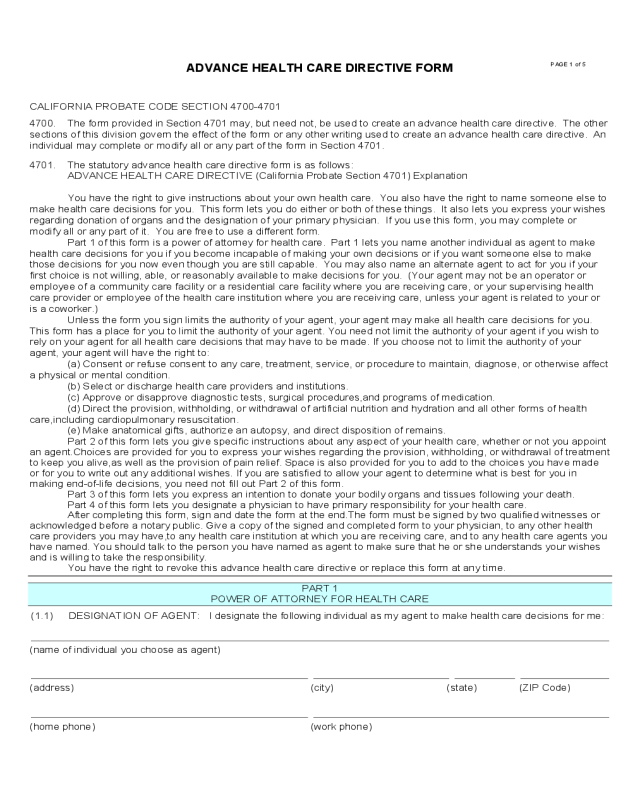
Health Insurance Claim Form. Beacon Health Options Mental HealthSubstance Abuse Treatment Claim Form. Beacon Health Options of Pennsylvania Attention.
Please be sure that as much of Part II is completed as possible. HEALTH INSURANCE CLAIM FORM New York State Government Employees Health Insurance Program APPROVED BY NATIONAL UNIFORM CLAIM COMMITTEE 0805 Please submit claims to. Beacon health empire plan claim form.
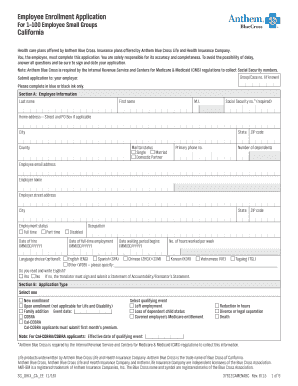
Beacon Health Options. You may also fill out and submit an online form on the Achieve Solutions website. Does your organization have secondarymultiple locations.
If you are unable to get the signature of the provider please print hisher name in Box 7 Part II. Create an account using your email or sign in via Google or Facebook. Please submit claims to.
CMI Beacon Health Claim Form 0221f. APPROVED BY NATIONAL UNIFORM CLAIM COMMITTEE 0805. MEDICARE MEDICAID TRICARE FECHAMPVA CHAMPUS.
Locate this form here. Upload the PDF you need to e-sign. All Mens Health Womens Health Vitamin Popular Searched Wayne county health department in wayne wv Healthy botanicals cbd oils Community health jobs seattle Atc healthcare services of georgia.
Beacon Health Options 200 State Street Boston MA 02109 Tel. What type of claim form will your organization file UB-04 formerly UB-82UB-92 Facility CMS-1500 billed by professional Both UB-04 and CMS-1500. Frequently Asked Questions PDF Resources.
Health Claim Form Its time for your check up. Beacon Health Options of California Inc ValueOptions of Kansas Inc CHCS IPA Inc. The Beacon Health Options North Carolina Engagement Center NCEC in Research Triangle Park has been part of the mental health and substance abuse services delivery system in North Carolina since 1992.
Please use the form below to submit your claim. Do that by pulling it from your internal storage or the cloud. Timely Filing Committee PO.
Submit this form for mental healthsubstance abuse treatment claims. For purposes of this handbook references to Beacon shall mean individually or collectively as applicable the Beacon legal entity with whom the provider has. EDI Claim Submission.
Autorización para que Beacon Health Options Opciones de Salud de Beacon divulgue información confidencial. Box 1800 Latham NY 12110 PICA PICA 1. TO BE COMPLETED BY EMPLOYEE INSURED.
Tips for Completing the CMS 1500. State Health Plan PPO Beginning in October 2006 Beacon. Hicksville NY 11802.
You will need to submit a completed Account Request Form. Beacon Health Credentialing Policies Official credentialing policies and procedures for contracted network providers to participate in the Beacon Health provider network. Sample Member Claims Form.
New Providers MD DO NP to be included under a new or existing contract. To sign a beacon health options claim form right from your iPhone or iPad just follow these brief guidelines. Claims must be submitted within 90 days of being incurred and original receiptsitemized bills must be attached.
Download your claim form here and have your doctor complete itDont worry be happy. Claim form Beacon requires that they complete Box 7 under Part II. Are all subsidiaries of Beacon Health Options Inc.
O Beacon claim number if previously billed o Outstanding amount o County of member A claim form CMS-1500 or UB-04 for claims not on file with Beacon with all required fields populated The Timely Filing Waiver Request may be mailed to. M EDICARE MEDICAID TRICARE CHAMPVA CHAM PUS GROUP HEA LTH A N F CA B K U G OTH R 1a. New York State Government Employees Health Insurance Program.
Beacon Health Options PO. Install the signNow application on your iOS device. You may attach your providers custom claim form for our review.
If you are insured with us and there is only damage to your windscreen Beacon will restore your visibility quickly.

/1095-BHealthCoverage-1-c2b35a65cb7046028b47940d68f4260c.png)