Mobile PDR is the OFFICIAL drug information app from PDR allowing healthcare professionals FREE access to the current drug prescribing information available. Drug Interaction Checker.
PDR drug identification guide.
Pdr medication look up. Over 11500 drug images updated. Use the pill finder to identify medications by visual appearance or medicine name. Theres a good chance that our Pill Identification Wizard Pill Finder can help you match the imprint size shape or color and lead you to the detailed description in our drug database.
It follows guidelines of the FDA regulations. Add a full drug regimen and view interactions. Nine times out of 10 its like Ive never heard of this drug when the calls over I would research it.
Brand Name Generic Name Classification Indication Use Contraindications Drug Form Side Effects Zantac Ranitidine H2 blocker Heartburn Porphyria Tablet Constipation nausea vomiting abdominal pain headache irregular heartbeat pneumonia dizziness liver problems rash blood cell changes possible allergic reaction including anaphylaxis trouble breathing swelling of airway Xanax Alprazolam Benzodiazepine Anxiety disorders panic disorders Known sensitivity to this drug. Periodically check your medicine cabinets for expired re-bottled or unidentified pills. Prescription drug pictures are categorized by form shape color and text imprint which you select using drop-down boxes.
Use the search field above to look up prescription or OTC drugs and herbal supplements. Id open up my PDR just to learn about this drug. And we would have to chart all of that down.
MA1520 - Pharmacology Look up Medication in a Drug Reference Resource Using the medications listed under. Drug recalls are actions taken by a firm to remove a product from the market and may be conducted on a firms own initiative by FDA request. PDR provides the following FDA-approved services including full prescribing information drug summaries FDA Early Warning Communications FDA Drug Safety Communications PDR Drug Alerts Medication Guides and free Continuing Medical Education CME course credits.
FDA provides a searchable list of recalled products. As a general rule. The easiest way to lookup drug information identify pills check interactions and set up your own personal medication records.
View all PDR Drug Communications including Drug Alerts Recalls and Approvals. View Homework Help - PDR Exercise part 1docx from MA 1520 at Charter College Vancouver. All fields are optional.
Search for the imprint first then refine by color andor shape if you have too many results. The final drug pictures are presented accompanied by helpful information including the drugs generic name brand name strength imprint and manufacturer. Available for Android and iOS devices.
MA1520 - Pharmacology Look up Medication in a Drug Reference Resource Using the medications listed under Brand name below look Study Resources. We would pick up patients from time to time and they might have a laundry list of meds. Fast and easy to use mobile PDR employs a simple but powerful search tool with access to thousands of drug summaries continually updated by PDR within a week of manufacturers updates.
Drug Pictures The Pill Identification Wizard is easy to use. Select pill color Select color --------- White --------- Beige Black Blue Brown Clear Gold Gray Green Maroon Orange Peach Pink Purple. Browse PDRs full list of drug information alphabetically by choosing the first letter of the drug you are tying to locate.
View PDR exercisedocx from MA 1520 at Charter College Anchorage. Use our comprehensive pill identifier to quickly and easily identify pills by imprint shape color or drug name. All therapeutic areas and medical specialties are covered within the PDR drug app including diabetes drugs pain drugs asthma and allergy drugs cardiovascular drugs obesity drugs cholesterol drugs psychiatric and mental health drugs pediatric drugs oncology drugs vaccines and biologics and more.
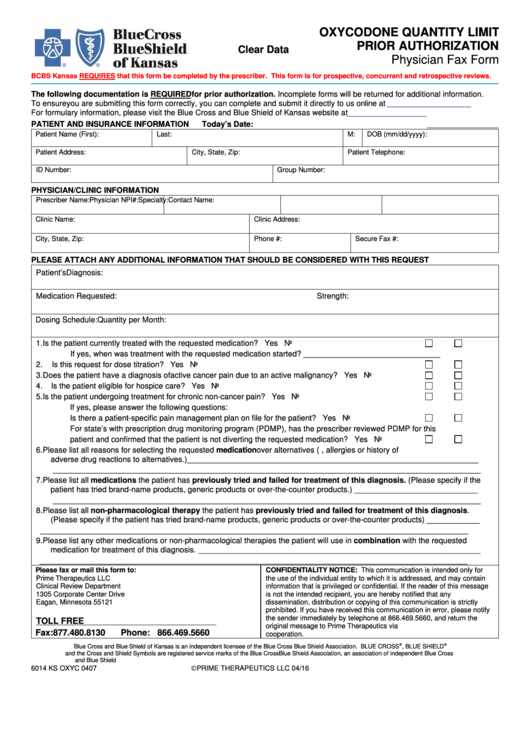
The information in the PDR which is similar to drug inserts isnt meant as a medical standard care. This information is required for all.