Thats why its always best to get fully covered with dental implant insurance. Services they cover include dental implants dentures braces X-Rays root.
 Does Dental Insurance Cover Implants All You Need To Know
Does Dental Insurance Cover Implants All You Need To Know
But keep in mind that any plan payments will only be a certain percentage of the total cost so youll still need to come up with additional funds.

Best dental coverage for implants. A dental insurance plan for an individual with 1200 in coverage the first year 2500 in. Some of Deltas plans do cover implants up to 50 but with certain restrictions. At EasyDentalQuotes we recommend you consider a plan with no waiting periods and coverage for dental implants such as one with Renaissance Dental.
This process takes time and having the best dental implant insurance or plan is very important. It can although dental insurance isnt always the best option for reducing dental implant costs. Your new tooth will look and feel just like your surrounding teeth.
Unlike other restorations a single tooth dental implant replaces your entire missing tooth from root to crown. Basic dental treatments like tooth extractions fillings root canals and gum disease treatment may be covered at a lower rate approximately 80 or less. Does Aetna Dental Insurance Cover Dental Implants.
While dental implants arent usually covered in the plans if your dentist recommends them he or she should send in the treatment plan and x-rays to Delta for a predetermination of coverage. It may also include payment options for the amount youre responsible for. Dental crowns dentures and dental implants are major procedures that tend to be covered at the lowest percentage such as 50.
The reason for the implant. However your Aetna policy may cover costs related to dentures crowns or related procedures. Dental implant insurance plans with no waiting periods and annual maximum coverage up to 3500.
There are certain insurance companies that offer plans with implant coverage such as Cigna Delta and others but these plans also often come with high deductibles or limits and exclusions that leave the consumer with a hefty price to pay. Although the CDG does not pay the full cost. A great benefit of getting a dental implant is that they have a success rate of up to 98 and with proper care they can last a lifetime.
This is a policy that will fully cover any cost incurred by a dental implant surgery. DeltaCare USA enrollees dont have. Top 10 Dental clinics hospitals for Dental Implants supported dentures.
6 Aon Dental Solutions Aon Dental Solutions has a small network of dentists around 15000 with discount plans starting at 125 per year for individuals and 180 per year for families. But you will need to ask for a pre-treatment estimate first. Most dental plans wont cover implant surgery although it is often available as an additional policy for an inflated premium.
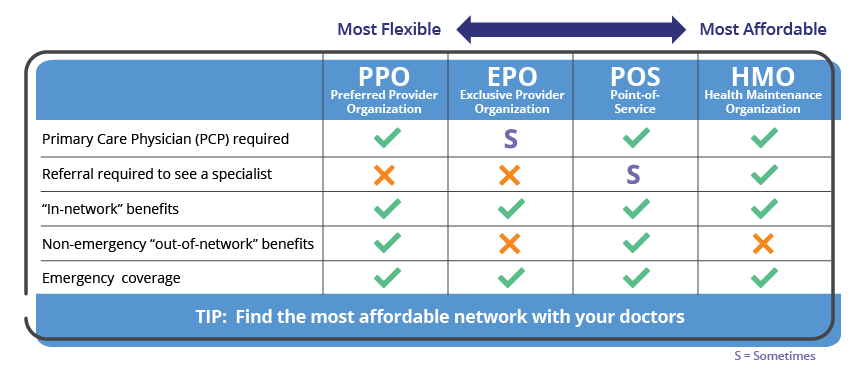
The pre-treatment estimate explains what your plan covers including whether you will exceed your maximum. THE SIMPLY INSURANCE WAY Dental Insurance made easy. Health insurance dental insurance or a combination of both may cover dental implants.
If you have one missing tooth or multiple that are not adjacent to each other then a single tooth dental implant may be your best. They serve as a replacement for your actual tooth root so they work and feel like natural teeth and are meant to last decades or even a lifetime. Compare dental clinic quality apples-to.
Thats where the next steps come in. Most dental insurance companies consider dental implants to be a cosmetic procedure which isnt covered by most policies. Show map About Dental Clinics See the best rated dentists specializing on dental implants supported dentures dental clinics in.
That being said dental implants are the best way to replace missing teeth. But since implants. Coverage depends on a couple of factors including.
Spirit Dental Vision offers coverage that includes dental implants as well as other major services. 9 While plan details vary from state to state Delta Dental offers several different types of. You may qualify for dental implants coverage with a Delta Dental PPO or Delta Dental Premier plan.
Instant online quotes for Dental Implant coverage - get quote from multiple companies so you know youre getting the best deal for your money. There are also other things that you should be thinking about before. What is Dental Implant Insurance.
What else you should know about Avia. Humana group dental plans are offered by Humana Insurance Company HumanaDental Insurance Company Humana Insurance Company of New York The Dental Concern Inc Humana Medical Plan of Utah Humana Health Benefit Plan of Louisiana Inc CompBenefits Company CompBenefits Insurance Company CompBenefits Dental Inc Humana Employers Health Plan of. Which dental insurance is best for implantsHow can I get free dental implantsThe Cosmetic Dentistry Program CDG provides partial subsidies to people in need of cosmetic services such as dental implants.
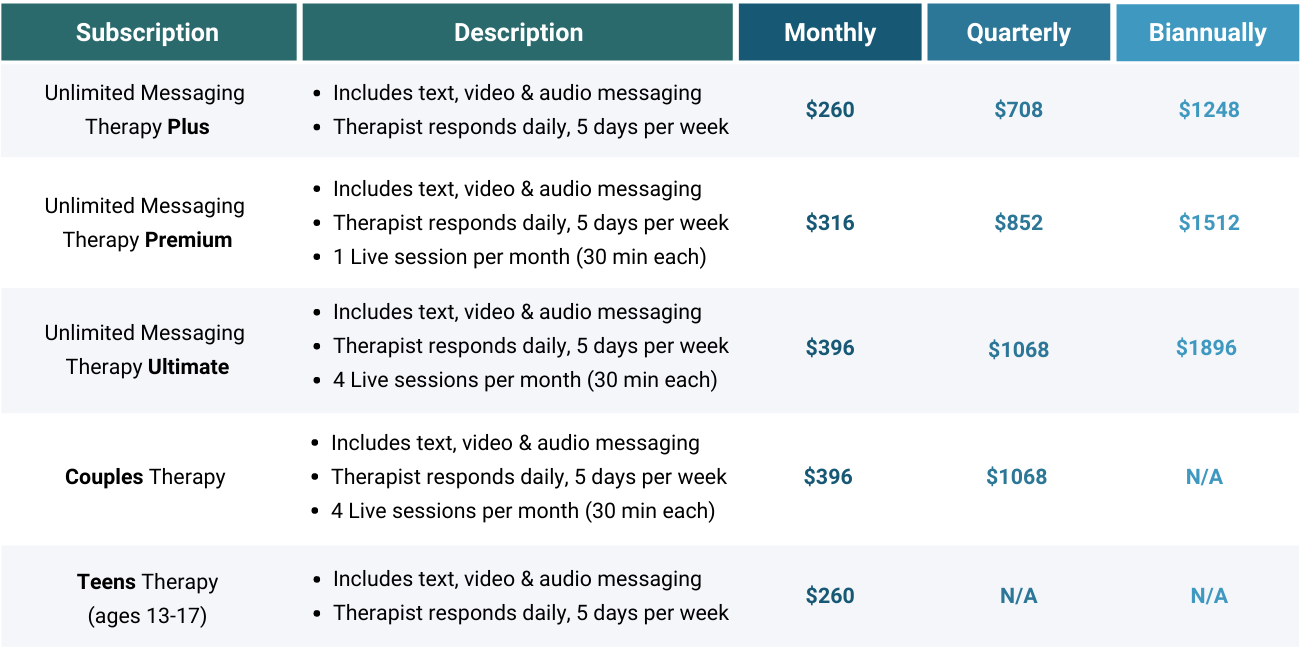
Dental Implant Insurance plans start as low as 1899 a month to fit anybodys budget. Delta Dental also boasts an A rating from AM Besta testament to the financial strength of the company.












/medicare-part-d-overview-4589766-ec01f6e5f22546d8b45249a54d466e53.png)