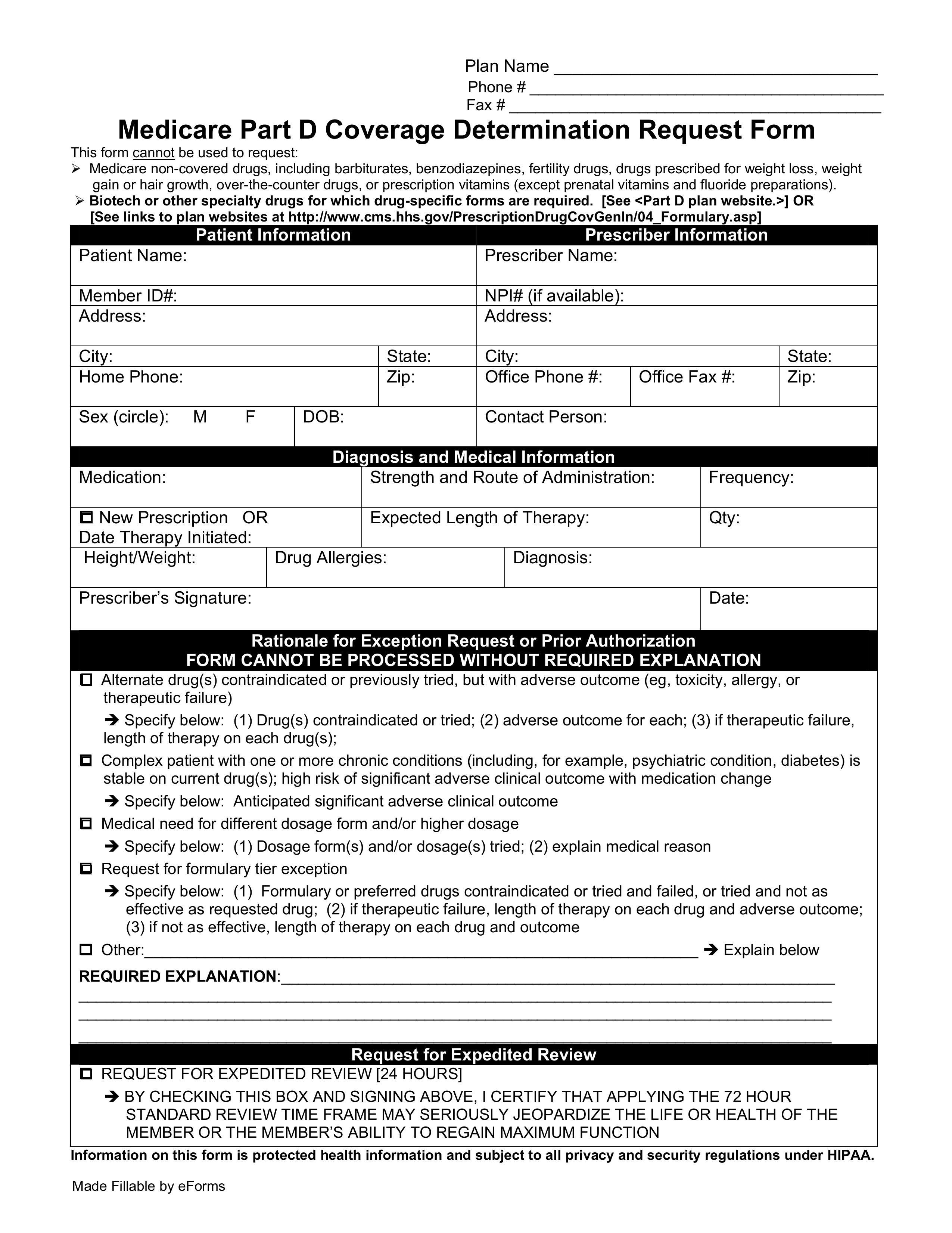
Pregnancy care does not require a Pre-Authorization. For Outpatient rehabilitation use the Medicare Advantage Outpatient Pre-Treatment Authorization Program Form.
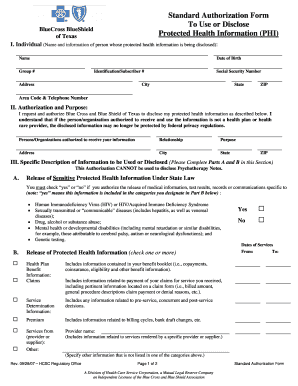
 Fillable Online Prior Authorization Request Carefirst Bluecross Blueshield Fax Email Print Pdffiller
Fillable Online Prior Authorization Request Carefirst Bluecross Blueshield Fax Email Print Pdffiller
Treatment Authorization Request OutPt Services ResidentialBH.
Carefirst prior authorization. For elective procedures where authorizations have already been submitted CareFirst will honor those initial authorizations which have been approved and maintain them in an approved status for up to 12 months pending member eligibility. Obstetrical Authorizations Notifications PDF Additional Forms. Contact 866-773-2884 for authorization regarding treatment.
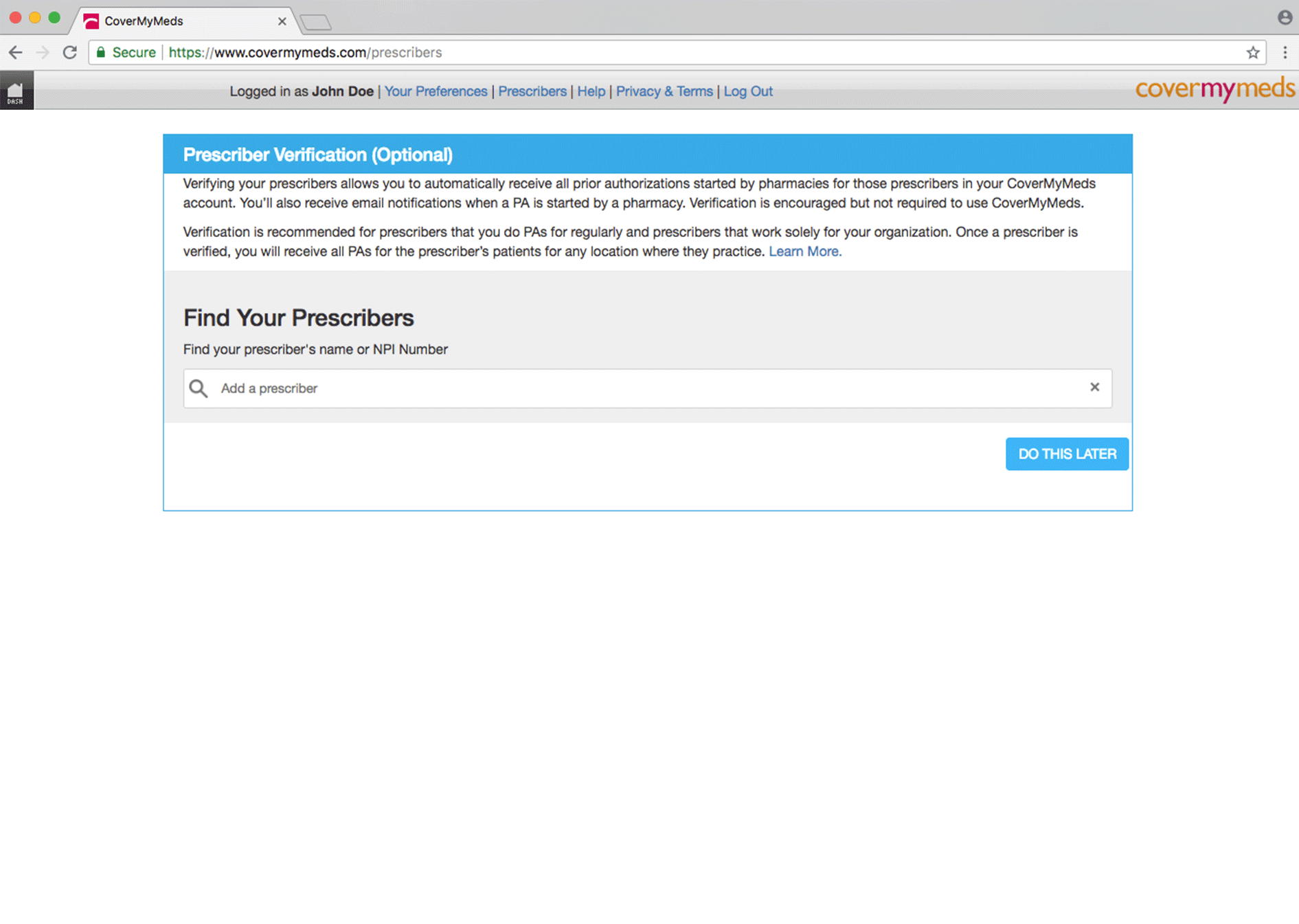
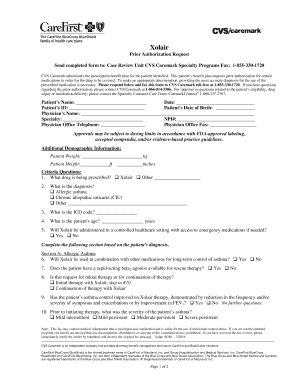
Prior authorization is required for elective surgeries. Prior Authorization Form CAREFIRST Subsys This fax machine is located in a secure location as required by HIPAA regulations. Drug Prior Authorization Prior authorization requests must be submitted electronically through the CareFirst Provider Portal for all drugs requiring prior authorization.
You may fax this OB Authorization form to UM at 202 821-1098. Please contact CVSCaremark at 1-855-582-2022 with questions regarding the. For Alpha Numeric codes use only the 1st Five numbers no alpha digitsmodifiers.
Completereview information sign and date. Enter your CPT Code. Prior to rendering the authorized service the health care practitioner must verify the members eligibility and benefits with CareFirst see page 2 for instructions.
The OBGYN is responsible for notifying the CareFirst CHPDCAlere Case Manager at 202 821-1100 for assistance with support services needed to help the pregnant enrollee during pregnancy. Prior authorization requests for drugs covered under the medical benefit must be submitted electronically through the CareFirst Provider Portal. Effective February 1 2019 CareFirst will require ordering physicians to request prior authorization for molecular genetic tests.
You must get this approval before you receive the service. View patients eligibility status and benefit information. This authorization does not guarantee payment of claim.
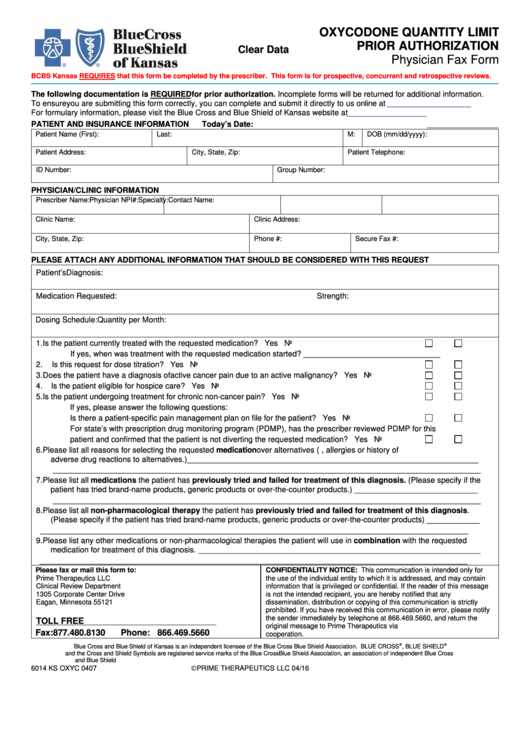
If the patients benefits are not covered on the date the authorized service is. To determine if prior authorization is required please enter the 5-digit CPT code below. Long-acting or Extended-release opioids fentanyl and methadone for moderate-to-severe pain.
Fax signed forms to CVSCaremark at 1-888-836-0730. When surgeries are rescheduled it will be the responsibility of the provider to contact the CareFirst. With questions regarding the prior authorization process.
Please contact CVSCaremark at. However plan notification of OB services is required. Please refer to the criteria listed below for genetic testing.
This fax machine is located in a secure location as required by HIPAA regulations. Ph 6027781800 Options 5 6 Fax 6027781838 For AdmissionsSNF send Facesheet to. Prior authorization or prior approval means approval for a health service that is not routinely covered by CareFirst CHPDC.
Prior Authorization is not needed for Pregnancy related care however notification is required. For services that require prior elevated nursemedical review only. It is only by partnering with providers such as yourself that we can truly achieve those goals.
You may fax the OB Prior Authorization form to the UM department at 202 821-1098. HSUM15 MAY PHOTOCOPY FOR OFFICE USE PREAUTHORIZATION. Prior Authorization Criteria Care1st uses clinically sound nationally developed and accepted criteria for making medical necessity decisions.
Please complete and submit a separate authorization form indicating measurable short-term and long-term goals for the member. Wellness care and diagnostic services such as screenings. To submit a prior authorization request online log in to the Provider Portal and navigate to the Pre-AuthNotifications tab.
Effective July 1 2017 CareFirst Community Health Plan Maryland CareFirst CHPMD requires a PRIOR AUTHORIZATION PA for 6 months unless indicated otherwise for certain opioid prescriptions as described below. Fax 6027788386 AHCCCS DDD ONECare Routine Urgent May seriously jeopardize members life health or function level Retroactive Patient Information Member Name. At CareFirst CHPDC we stand by our providers in offering exceptional health care to DC locals and their families.
Clinical criteria utilized in decision making include but is not limited to. Access the Provider Portal to. You may enter multiple codes up to 5.
SERVICES ARE NOT CONSIDERED AUTHORIZED UNTIL CAREFIRST BLUECROSS BLUESHIELD MEDICARE ADVANTAGE ISSUES AN APPROVAL. All authorizations are subject to eligibility requirements and benefit plan limitations. Fax signed forms to CVSCaremark at.
OB care and services will be coordinated by a CareFirst CHPDC OB Case Manager. Prior Authorization Form CareFirst Global Post Step Therapy State of Maryland Mandate REG HMF Completereview information sign and date. AHCCCS Guidelines DDD Criteria.