MVP Health Plan Inc. Coverage Determination Guidelines may address such matters as whether services are skilled versus custodial or reconstructive versus cosmetic.
 Medicare Part B Local Coverage Determinations Lcds Download Table
Medicare Part B Local Coverage Determinations Lcds Download Table
In some cases UnitedHealthcare may decide a drug isnt covered or is no longer covered by Medicare for you.
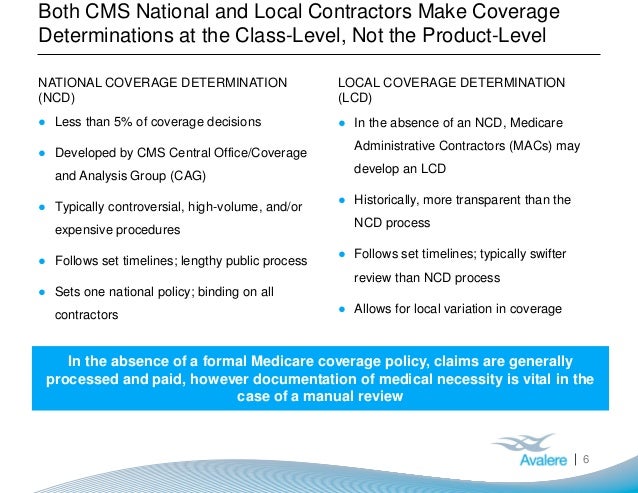
Coverage determination medicare. In most cases the standard for receiving an exemption for a non-covered expense is if the medication or procedure is deemed medically necessary by your physician and your doctor has documented. Whether a certain drug is covered Whether you have met the requirements to get a requested drug. Local coverage determinations LCDs and national coverage determinations NCDs are coverage and payment guideline documents published by The Centers for Medicare and Medicaid Services CMS or their administrative contractors.
Your Medicare Part D plan covers many of. Whats a Local Coverage Determination LCD. NATIONAL OR LOCAL COVERAGE DETERMINATIONS.
When this happens CMS issues a National Coverage Determination NCD. Often a coverage determination is the first step in the Medicare appeals process. An Organization Determination is needed only when the service being requested is sometimes covered by Medicare based on medical necessity requirements and you do not feel the member will meet criteria.
Receipt of or payment for a prescription drug that an enrollee believes may be covered. 57 Zeilen Local coverage determinations LCDS are defined in Section. Specifically LCDs are published by Medicare Administrative Contractors MACs and generally apply to beneficiaries.
Clinicians who bill Medicare should. MACs determine which types of interventions are covered along with documentation needed to justify medical necessity utilization guidelines frequency allowed etc. Coverage Determinations and Redeterminations for Drugs A coverage determination is a decision about whether a drug prescribed for you will be covered by us and the amount youll need to pay.
Coverage Determinations You can ask MVP to cover a drug for a lower cost remove an additional requirement or limit or cover a drug that is not listed on the Formulary. 131 Zeilen The information contained herein is applicable where appropriate to all DME. You can ask us to cover.
If your coverage determination fails to get the result you desired dont worry. CMS IOM Publication 100-03 Medicare National Coverage Determinations NCD Manual Chapter 1 Part 2 Section 1402 Breast Reconstruction Following Mastectomy and Section 1404 Plastic Surgery to Correct Moon Face. The Centers for Medicare Medicaid Services CMS sometimes change the coverage rules that apply to an item or service.
You can get help with this process through Medicaregov. How do I Request a Coverage Determination. Dermal Injections for the Treatment of Facila Lipodystrophy Syndrome LDS.
There you can learn to how appoint a representative to guide you through the process. A tiering or formulary exception request for more information about exceptions click on the link to Exceptions located on the left hand side of this page. Enrollment in MVP Health Plan depends on contract renewal.
Part 4 Section 2505. What benefits and services are changing. A coverage determination is the first decision made by your Medicare drug plan not the pharmacy about your Benefits Glossary including these.
Every year Medicare evaluates plans based on a 5-star rating system. LCDs are decisions made by a Medicare Administrative Contractor MAC whether to cover a particular item or service in a MACs jurisdiction region in accordance with section 1862 a 1 A of the Social Security Act. A coverage determination coverage decision is a decision UnitedHealthcare makes about your benefits and coverage or about the amount UnitedHealthcare pays for your prescription drugs under the Part D benefit in your plan.
A coverage determination is the decision process used to receive access to medications or medical procedures that may not usually covered by Medicare. Medicare coverage for many tests items and services depends on where you live. What benefits and services are covered.
The map below shows the Medicare Part AB Medicare Administrative Contractors MAC Jurisdictions. MACs are Medicare contractors that develop LCDs and process Medicare claims. If a drug is not covered or there are restrictions or limits on a drug you may request a coverage determination.
This process is called a coverage determination. Is an HMO-POSPPOMSA organization with a Medicare contract. This list only includes tests items and services both covered and non-covered if coverage is the same no matter where you live.
Use this list if youre a person with Medicare family member or caregiver. Coverage Determination Guidelines are used to determine whether a service falls within a benefit category or is excluded from coverage. A coverage determination is any decision made by the Part D plan sponsor regarding.
