Peer to Peer Scheduling Request Form- UnitedHealthcare offers the opportunity for your physician to speak with our medical director to discuss the medical policy and documentation requirements which determined the response for your prior authorization or concurrent review request. And click on the Link button in the top right corner.
Https Www Uhcprovider Com Content Dam Provider Docs Public Prior Auth Uhccp Pharmacy Forms H L Upc Humira Prior Authorization Form Pdf
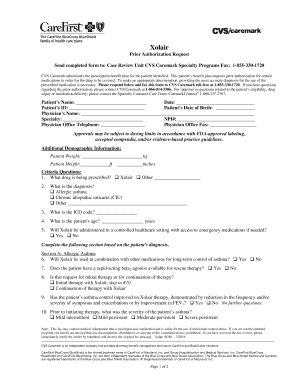
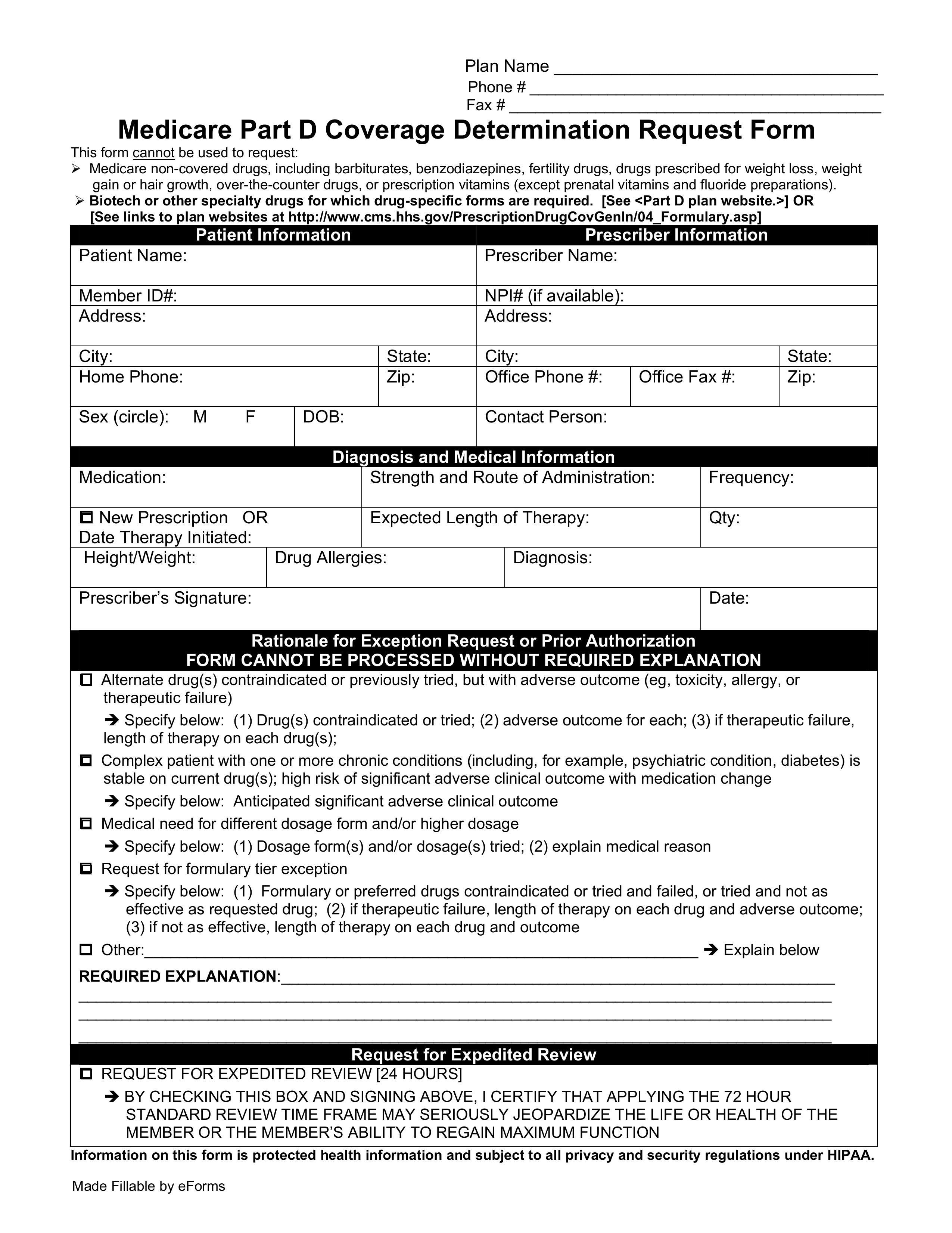
The purpose of this form is to demonstrate medical justification for prescribing the drug in question when other drugs on the PDL might serve the same purpose.
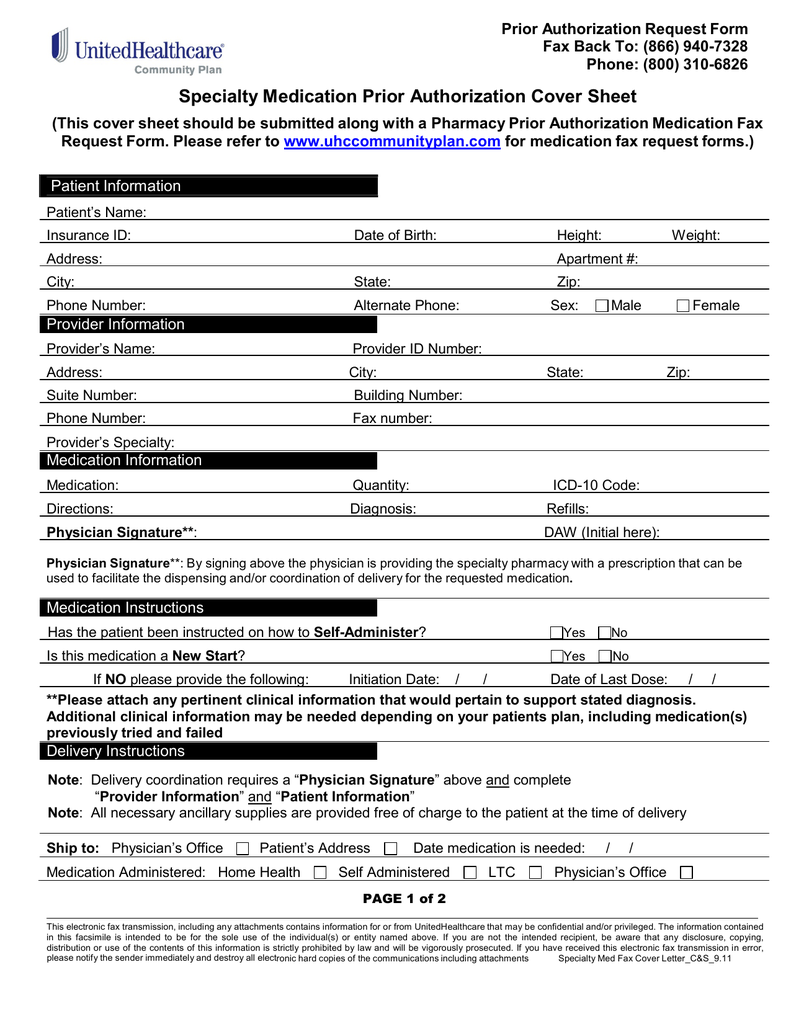
Unitedhealthcare medication prior authorization form. Medication Prior Authorization Request Form - Medication Prior Authorization Request Form Opens in a new tab pdf 25483KB Last Updated. If your facility doesnt use EDI our online Prior. To simplify your experience with prior authorization and save time please submit your prior authorization request through the following online portals.
This form may contain multiple pages. If a prior authorization is denied you may be responsible for the cost of. You may also initiate your request by phone by calling the number on.
Upload clinical notes or attach medical records and images to a request. UnitedHealthcares home for Care Provider information with 247 access to Link self-service tools medical policies news bulletins and great resources to support administrative tasks including eligibility claims and prior authorizations. Unitedhealthcare prior auth form for medication In this section you will find the tools and resources you need to help manage your practices prior authorization and notification requirements with program specific information available for Cardiology Oncology Radiology Clinical Pharmacy and Specialty Drugs.
Use the Prior Authorization and Notification tool on Link. Your doctor is responsible for getting a prior authorization. Fax us a Pharmacy Prior Authorization Form.
They will provide us with the information needed. Be sure to use the prior authorization form for your. UnitedHealthcare offers two efficient electronic methods to submit admission notifications.
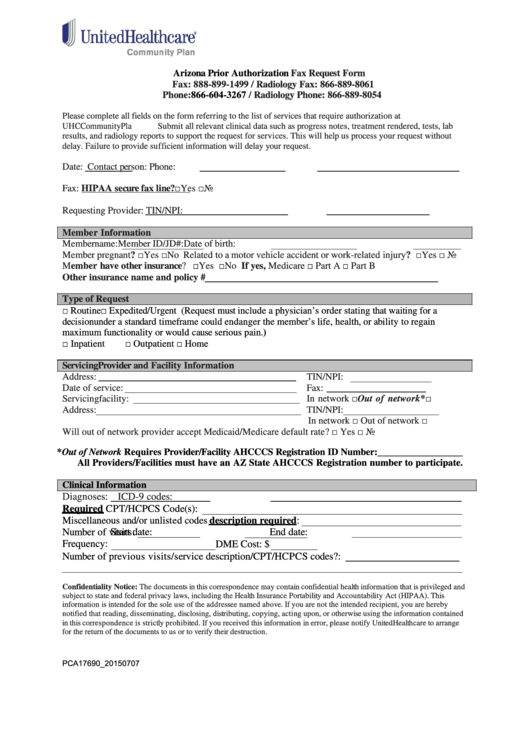
Any relevant clinical data and medical documents should also be attached with this form. Certain medications require specific documentation that cant be submitted by phone. Prior Authorization Request Form Please complete this entire form and fax it to.
Call the Pharmacy Prior Authorization Service at 800-310-6826. In some cases a physician may choose to prescribe medication that is not on the preferred drug list PDL and will have to fill out a UnitedHealthcare prior authorization form. This is called prior authorization.
877-842-3210 Notificationprior authorization is not required for emergency or urgent care. The form should be submitted to UHC where they will review the. 05042020 Prescription Redetermination Request Form.
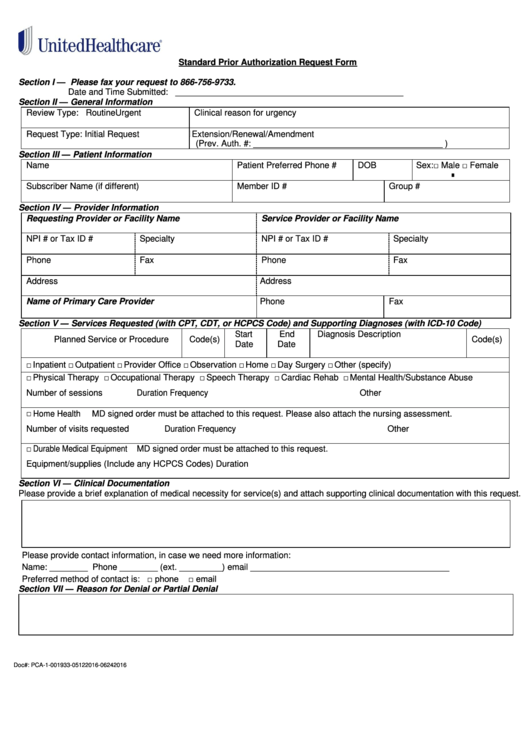
Standard Prior Authorization Request Form Please submit your request online using our Prior Authorization and Notification tool on Link. Standalone Direct Deposit form pdf. Electronic Prior Authorization ePA Submit an ePA using CoverMyMeds.
Prescription Redetermination Request Form - Prescription Redetermination Request Form Opens in a new tab pdf 5106KB Last Updated. On the prior authorization form the person making the request must provide a medical rationale as to why the chosen medication is necessary for the patient in question. Please complete all pages to avoid a delay in our decision.
If the patient has tried any preferred medications in treatment of the relevant diagnosis the duration of therapy and reason for failure will be described in the form as supporting justification for making this request. The electronic data interchange EDI HIPAA 278N transaction can be sent directly to UnitedHealthcare or through a clearinghouse in either batch or real-time format which can result in fewer late notifications and reimbursement penalties. Your primary UnitedHealthcare prior authorization resource the Prior.
Member Information Prescriber Information Member Name. If you have questions please call 800-310-6826. When you find the plan you may want to enroll in click the View Plan Details button to access your enrollment form.
UnitedHealthcare is an operating division of UnitedHealth Group the largest single health carrier in. Persons covered under a UnitedHealthcare. If a prior authorization is approved those services will be covered by your health plan.
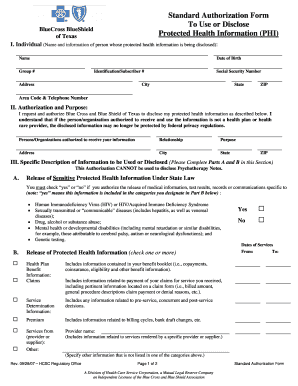
Unitedhealthcare medication prior authorization form 2020 pdf On February 26 2016 the FDA issued an Emergency Use Authorization EUA to authorize the emergency use of Centers for Disease Control and Preventions CDC Zika Immunoglobulin M IgM Antibody Capture Enzyme-Linked Immunosorbent Assay Zika MAC-ELISA for the. Submit a new request for medical prior authorization or to notify UnitedHealthcare of an inpatient admission. Standalone personal representative form pdf These optional forms are used by the member to provide UnitedHealthcare with authorization to discuss their claim with someone other than the member.
At UnitedHealthcare we are committed to improving the health care system. Allow at least 24 hours for review. Then select the Prior Authorization and Notification tool tile on your Link dashboard.
Check the status or update a previously submitted request for prior authorization or notification using the reference number or member or provider information. These may include opioids hepatitis C medications growth hormone Synagis and Enoxaparin Lovenox.