The Medicare Part D Transition and Emergency Fill Policy defines how Network Health Insurance Corporation NHIC or their delegate will provide a Transition Fill Process for Medicare Part D beneficiaries which allows certain members to obtain non -formulary Part D drugs or drugs subject to requirementslimits. Call us toll-free at 1-888-340-5504 TRS 711 8 am8 pm.
 Medicare Part D Transition Prior Authorization Exceptions Lis
Medicare Part D Transition Prior Authorization Exceptions Lis
Before switching to a different Part D plan either a stand-alone Part D plan PDP or.

Transition fill medicare. Federal law requires switching to Medicare at. You recently switched plans and your medication. Year to the next you may be eligible for a transition fill if the following applies to you.
Be eligible for a transition fill. A transition fill is a temporary 30-day prescription supply or refill of a non-formulary drug provided to. While you are using the temporary medication supply transition fill you and your physician can seek an.
The Delegated PBM transition fill policies are as follows. New to the prescription plan at the start of the contract year Newly eligible for Medicare Part D of the contract year Switching from one Medicare Part D plan to another after January 1st in the contract year. Transitioning from coverage through the Affordable Care Act Marketplace exchanges also is a common trip-up point.
If you receive Extra Help for your Medicare prescription drug coverage the copayments for transition supplies of medication will not exceed the current statutory maximum copayment amounts. People who have stayed with the same Medicare drug plan into the next year and now fi. Youll need to fill out part of it and your employer will need to fill out.
If you are currently taking drugs that are not listed in the plans drug list formulary from one year to the nest you may be eligible for a transition fill if the following applies to you. Transition Fill - Medicare TF. CMS L564 This is called the Request for Employer Information form.
If your medication is still a part of the Medicare program you can ask your Medicare prescription drug plan for. The Delegated PBM supports UUHIP in administering a transition process that is in compliance with the established CMS transition requirements. Transition Prescription Fill Process FirstMedicare Direct has a process in place to allow transition members to receive a supply of Part D drugs that may have coverage restrictions or are not on the FirstMedicare Direct covered drug list formulary.
Keep in mind that Medicare can only start on the first day of the month. Before switching to a different Part D plan either stand-alone or through a Medicare Advantage Plan Or before your current plan changed its coverage at the start of a new. Plans must provide a transition refill if one of these is true.
Millions of prescriptions are being filled every day with Medicare drug plans generally covering a broader range of. You can file a formulary exception with your. A temporary supply of a Part D covered drug per CMS Part D requirements.
Its important to understand how your current coverage works with Medicare. You may also be eligible for a one-time temporary 1-month supply if you qualify for an emergency fill while residing in a long-term care LTC facility after the first 90 days as a new member or you have encountered a level of care change. Can I ask my Medicare drug plan for a formulary exception before the start of the January coverage period.
As stated in regulation at 42 CFR 423120b3 and the current version of Chapter 6 of the Medicare Prescription Drug Benefit Manual D Part D sponsors must provide for an appropriate transition process for new enrollees and current enrollees prescribed Part D drugs that are not on its formulary. I have employer coverage and. Transition drug refills 2021 Medicare Rights Center Helpline.
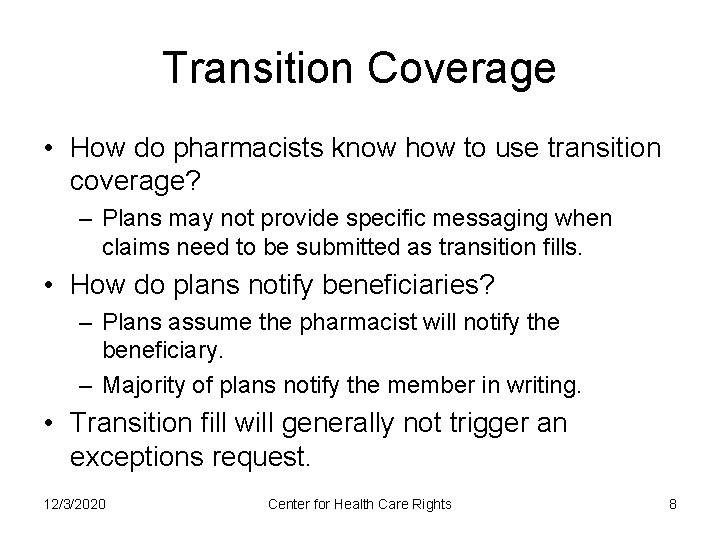
What is a transition fill. TRANSITION FACT SHEET Medicares highest priority is making sure that Part D beneficiaries have access to the drugs they need. If you have questions about your current insurance the best source of information is your benefits administrator insurer or plan provider.
A transition refill also called a transition fill is a one-time 30-day supply of a drug youve been taking that your plan doesnt cover. New to the prescription plan at the start of the contract year Newly eligible for Medicare Part D of the. A transition refill also known as a transition fill is typically a one-time 30-day supply of a drug that you were taking.
