Provider Preauthorization and Precertification Requirements - Blue Cross PPO and Medicare Plus Blue SM PPO PDF Northwood DMEPOS Management Program FAQ PDF. The services marked with an asterisk only require Pre-Service Review for members enrolled in BlueChoice products if performed in an outpatient setting that is on the campus of a hospital.
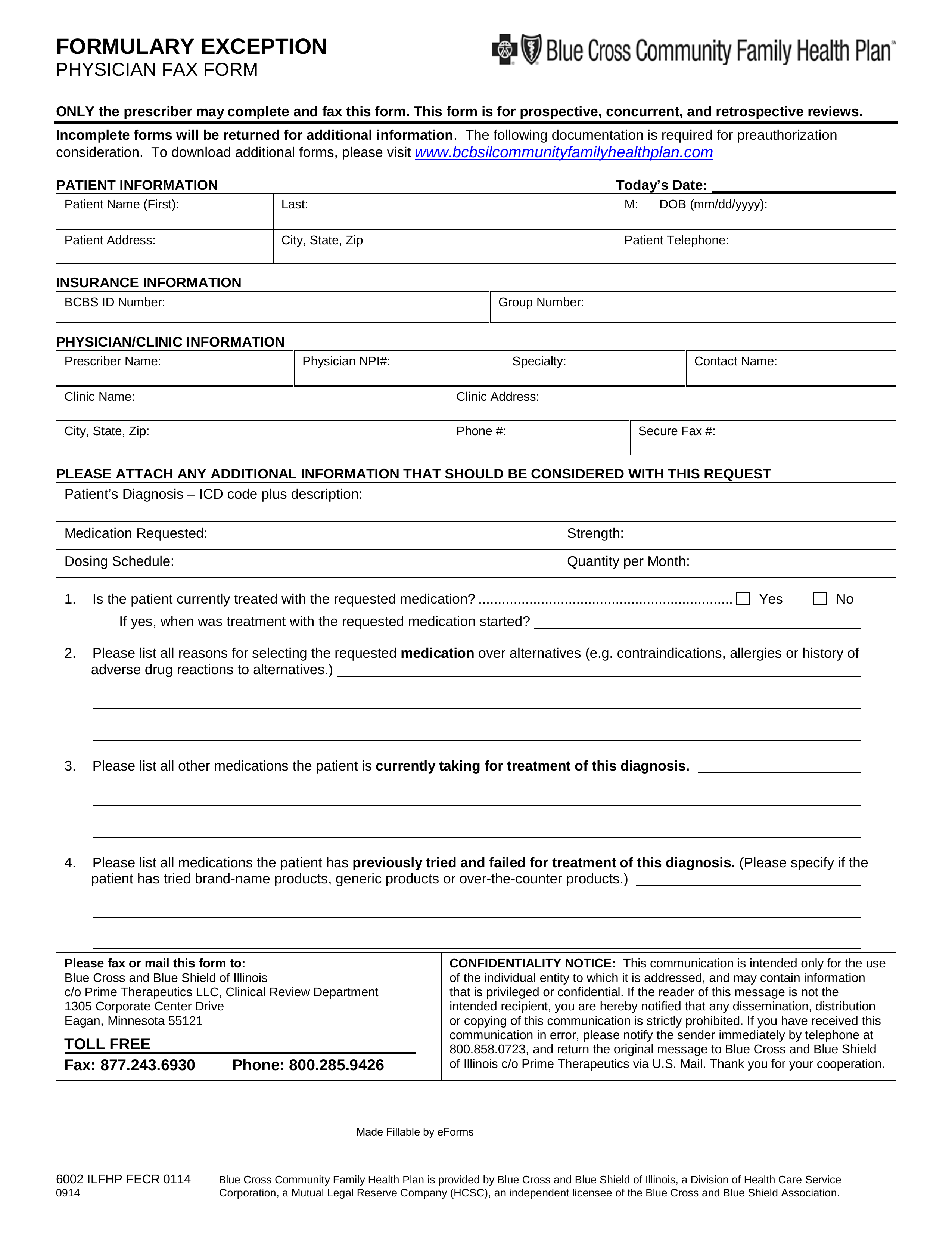 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
SM TM Registered and Service Marks.
Blue cross precertification. To find precertification information for Blue Cross Blue Shield members outside North Dakota enter the members three-character prefix in the box below. Premera Blue Cross is an independent licensee of the Blue Cross Blue Shield Association serving businesses and residents of Alaska and Washington state excluding Clark County. To determine if your employer plan is subject to these additional precertification requirements your benefit booklet will say the plan benefits are underwritten in the Administrative Section at the end of your benefit.
Premera Blue Cross complies with applicable federal civil rights laws and does not discriminate on the basis of race color national origin age disability or sex. Because you are still responsible for ensuring that your care is precertified you should always ask your provider if they have contacted us and provided all the necessary information. This applies to services performed on an elective non-emergency basis.
Medical and Pharmacy Services that Need Prior Authorization As part of your Florida Blue health coverage we provide services to help you save money by avoiding unnecessary costs. Precertification Request Availity LLC is an independent company providing administrative support services on behalf of Anthem Blue Cross and Blue Shield Healthcare Solutions. A few plans may continue to require prior authorization for mental health services.
Contact Companion Benefits Alternatives CBA to verify by calling 800-868-1032. In most cases your physician or facility will take care of requesting precertification. Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue Shield Association.
PPO outpatient services do not require Pre-Service Review. CBA is a separate company that administers mental health and substance abuse benefits on behalf of BlueCross BlueShield of South Carolina and BlueChoice HealthPlan. This webpage applies only to Blue Cross and Blue Shield of Alabama individual and family non-group plans and underwritten employer group plans.
Utilization Management Program and Precertification. Precertification approval decisions are based on information provided during the request process. Registered Marks of the Blue Cross and Blue Shield Association.
Some forms below can be submitted online. Premera Blue Cross complies with applicable federal civil rights laws and does not discriminate on the basis of race color national origin age disability or sex. To complete a precertification medical records might be required.
1996-Blue Cross Blue Shield of Michigan and Blue Care Network are nonprofit corporations and independent licensees of the Blue Cross and Blue Shield Association. Type of information being requested. To view the out-of-area Blue Plans medical policy or general pre-certificationpre-authorization information please select the type of information requested enter the first three letters of the members identification number on the Blue Cross Blue Shield ID card and click GO.
Inpatient services and nonparticipating providers always require prior authorization. We provide health. For Federal Employee Program FEP precertification requirements please see the separate FEP precertification list.
Prior Authorization Lookup Tool - Anthem Blue Cross Prior Authorization Lookup Tool Please verify benefit coverage prior to rendering services. Premera Blue Cross complies with applicable federal civil rights laws and does not discriminate on the basis of race color national origin age disability or sex. Although precertification may not be required for a particular service the claim for the service may still be subject to review for medical necessity as well as benefits limitations exclusions and waivers if applicable.
Pre-Certification The information presented here applies to most Blue Cross Blue Shield of Mississippi Members but there may be some differences based on each individuals health and wellness benefit plan. Services that require precertification As of January 1 2021 this list applies to all Independence Blue Cross HMO PPO and POS products including Flex products. When you and your doctor are making decisions about your health care and how your benefits will work we can help.
Premera Blue Cross is an independent licensee of the Blue Cross Blue Shield Association serving businesses and residents of Alaska and Washington state excluding Clark County. Member Prefix Enter the first three characters of members ID card.
