Give yourself the gift of clear vision. FEDVIP vision plans vary in coverage and cost.
 Vsp Vision Care Vision Insurance
Vsp Vision Care Vision Insurance
Business development activities initially focused on securing contracts with health plans.

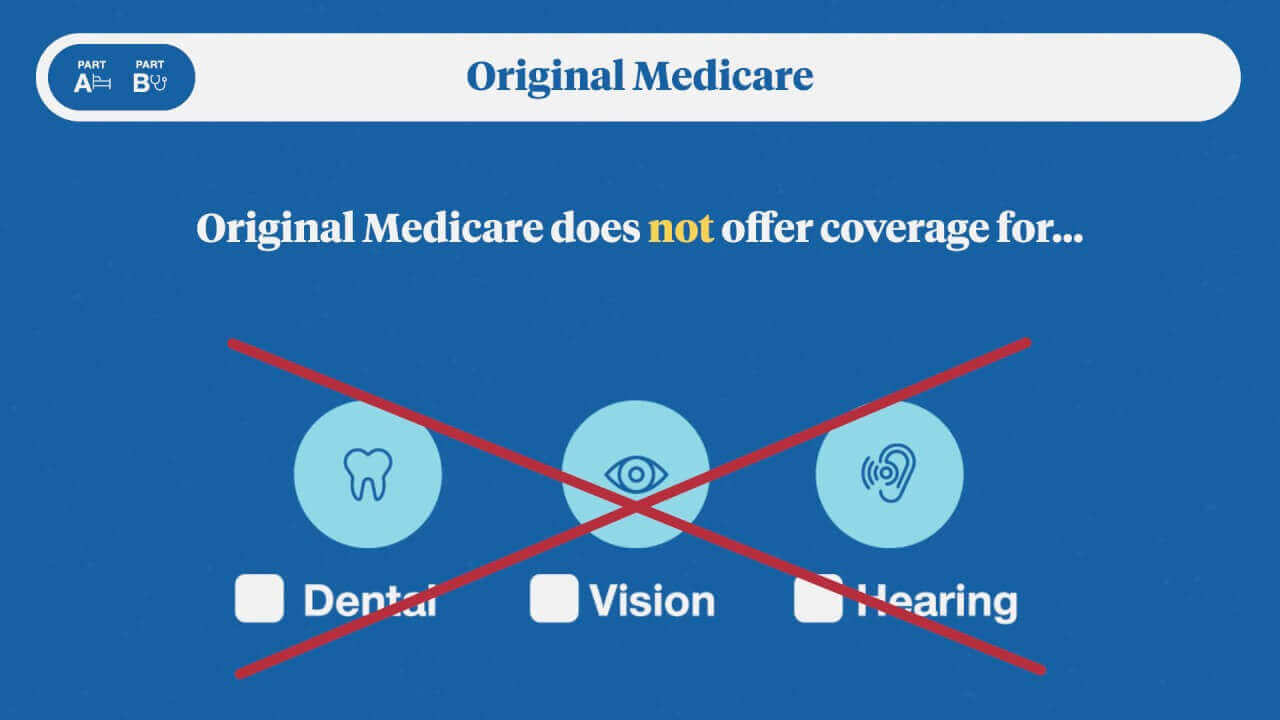
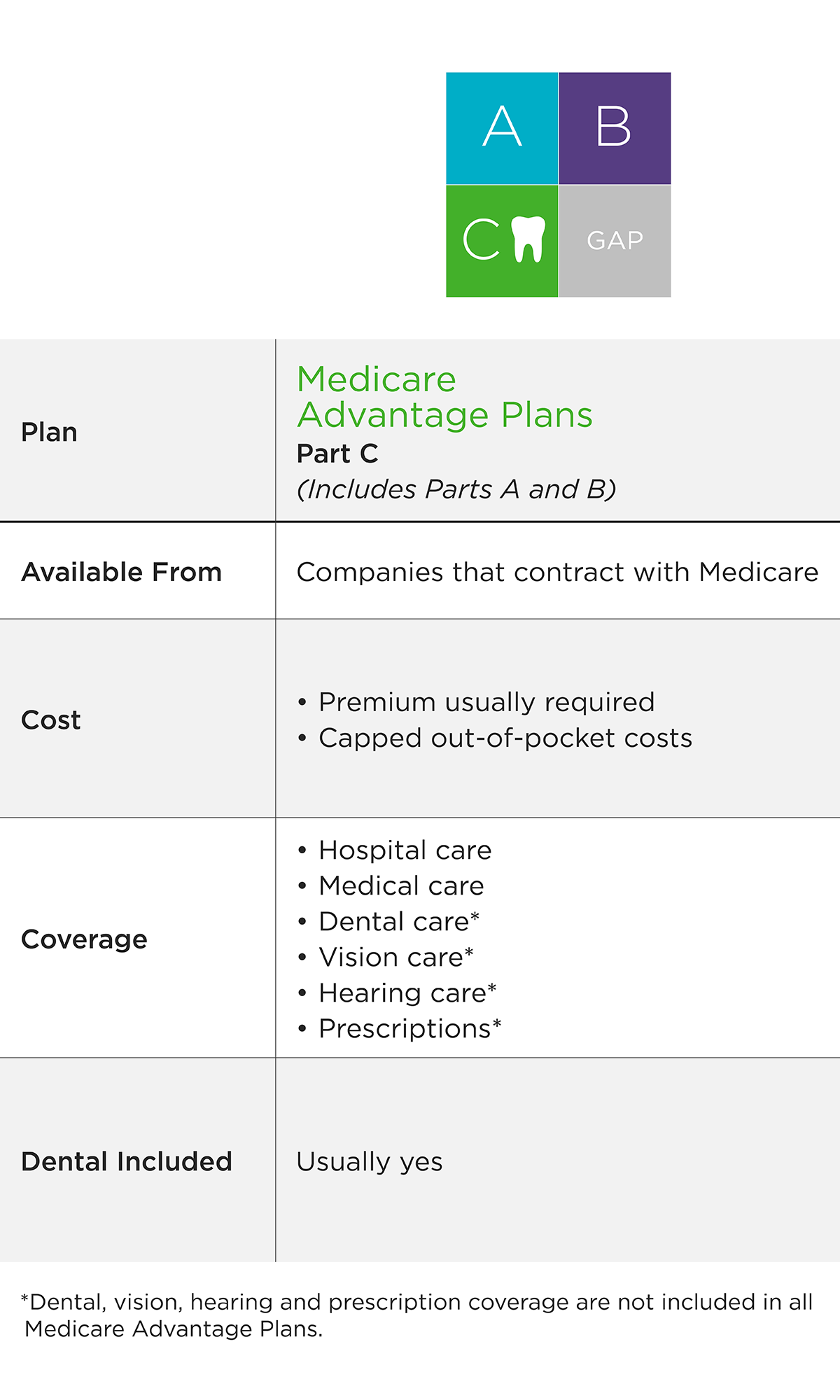
Vision care for life providers. However you do not need to select a primary care dentist. They may include routine eye exams eyeglasses and contact lenses. WellCard members can receive up to 50 in discounts and enjoy.
Paying out-of-pocket for necessary eye care can cost hundreds of dollars or more. We look for ways to help grow your practice and optimize lifetime value. EyeMed Vision Care LLC is an independent company that offers a vision provider.
At EyeMed our goal is to improve benefits in ways that are good for clients members independent eye care professionals and the industry as a whole. Full Life is working toward a future where adults with serious illnesses or disabilities can be supported in the community rather than living in isolation or needing to resort to institutional care. EyeMed plans pay for annual exams either at no cost or for a 10 deductible.
The MetLife Exclusive Provider Organization EPO contains features similar to PDP DHMO. Starting today providers of the most popular paramedical services and vision care can submit claims on behalf of plan members as soon as the service is provided. With more than 66000 provider access points nationwide youll enjoy immediate savings service and convenience.
Believe it is possible for everyone to find joy in life. Essilors social impact fund Vision For Life announced a 300000 financial support scheme to help over 1800 vulnerable primary vision care providers whose livelihoods are at risk due to the ongoing COVID-19 pandemic. Available in CA FL NJ NY TX.
Only the policy can provide the actual terms of coverage. Companion Life in association with EyeMed Vision Care offers easy access to thousands of conveniently located vision care providers including optometrists ophthalmologists opticians and many leading optical retailers such as LensCrafters Target Optical Sears Optical JCPenney Optical and Pearle Vision locations. The VSP Global Premier Program now includes thousands of private practice doctors and over 700 Visionworks locations nationwide making finding a doctor for your annual eye exam more convenient than ever.
These primary vision care providers are based in five countries India Bangladesh Indonesia Cambodia and Kenya and will each receive a. The Dearborn Group Vision Care policies referenced may not be available in all states. TRICARE For Life is the plan for you if.
Even if you have vision insurance WellCard can save your family on replacement glasses non-covered spare glasses designer sunglasses and more. The financial strength of Fidelity Security Life backs EyeMeds vision policies. 66 Deer Park Ave Babylon NY 11702-2802.
Never give up on people. Visibly also offers eye care providers eyewear retailers and other organizations customizable software solutions to enable better patient and consumer experiences. In 2000 the founders made the strategic decision to focus instead on employer-based vision benefits.
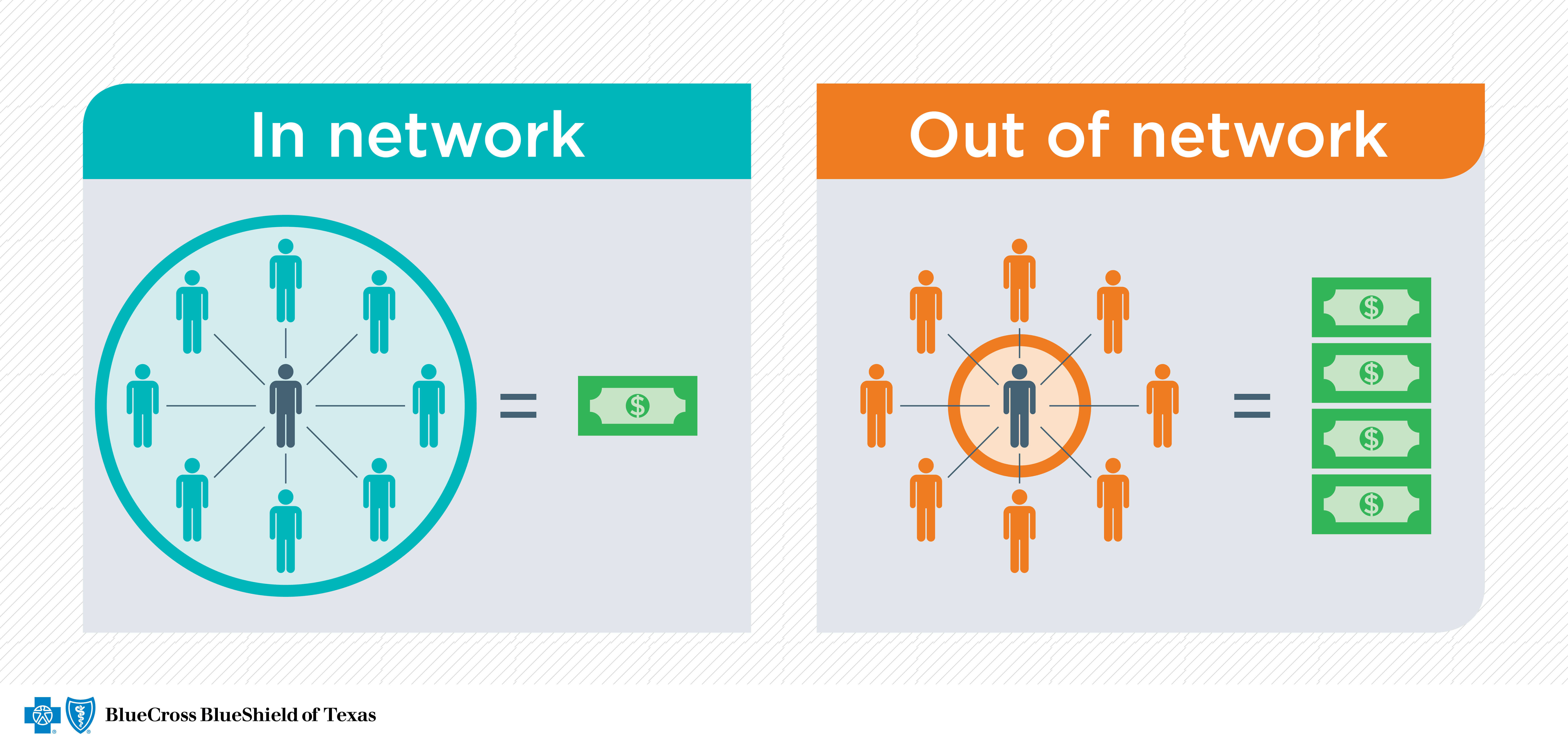
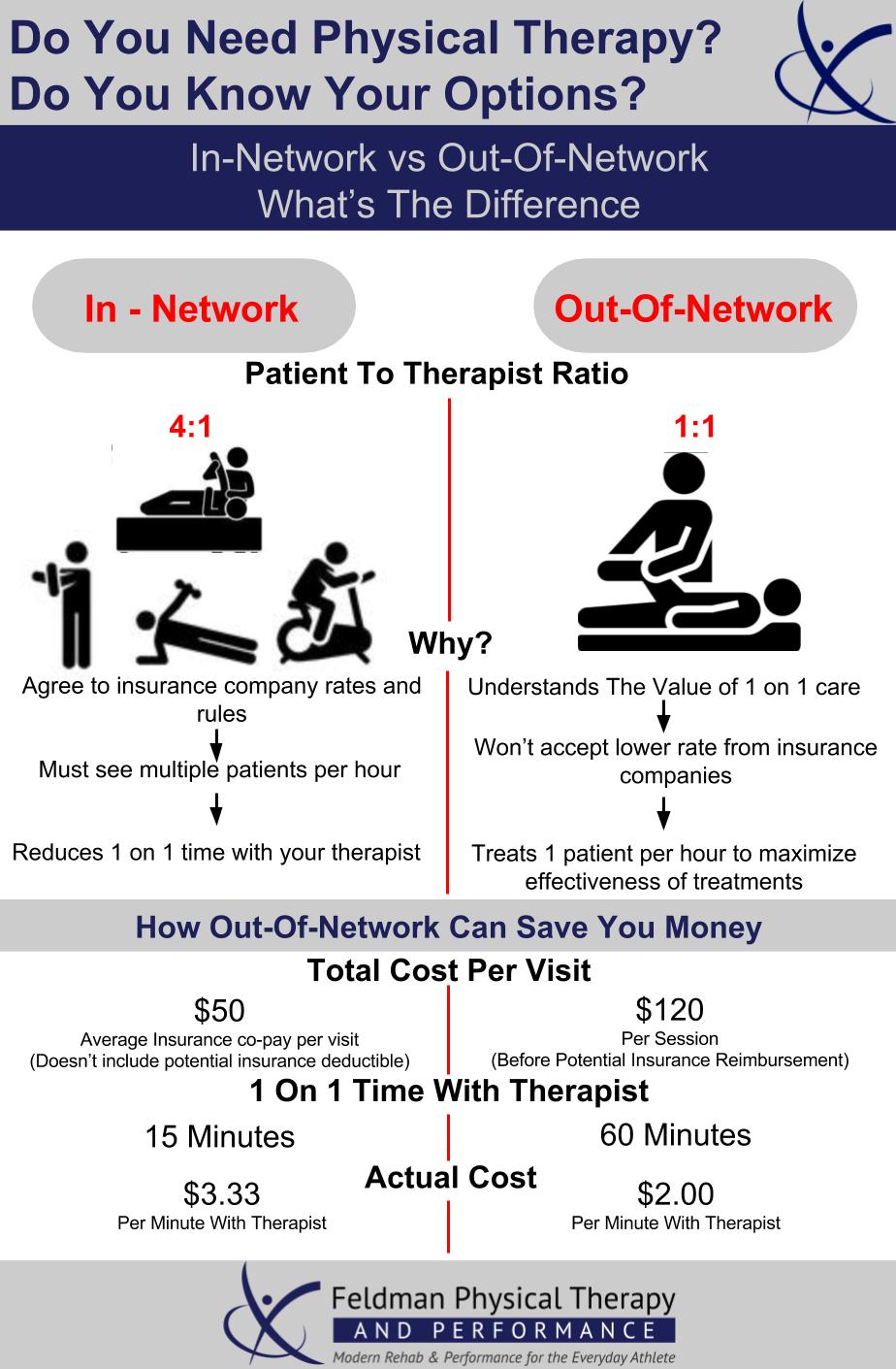
You must see an in-network EPO provider to utilize dental benefits. Empire Life has enhanced its eClaims suite of tools to make it faster and easier for plan members to get reimbursed for health care claim costs. Vision insurance can help cover the cost of care while providing valuable access to a network of.
However youll pay more if you get care from Veterans Administration providers or providers who opt-out of Medicare because theyre not allowed to bill Medicare. Coverage is available worldwide and you can see any provider you want. Visiblys vision is to create a world where eye care is available to anyone anywhere anytime.
Vision For Life Corp is a health care organization in Babylon with Optometrist listed as their primary medical specialization. All policies are subject to issue limitations exclusions and other coverage conditions. FIND MY PREMIER DOCTOR Vision Coverage for Every Stage of Life.
You have both Medicare Part A and B. Dearborn Group Vision Care benefits are underwritten by Dearborn Life Insurance Company. Over the years as the company has grown CECs mission has remained focused on offering the simplest vision plan ever designed.
Its mission to develop digital technologies that increase access and choice while partnering with doctors. The Vision Care Group of Companies has built a reputation as one of the best eye care solution providers in Sri Lanka by using an innovative approach and state-of-the-art equipment to ensure that customers receive world-class eye care. Vision insurance is designed to assist in covering necessary care for your eyes including preventive care such as regular exams or vision tests corrective lenses frames contacts and more.
We use advanced diagnostic technology and vision correction products and are committed to improving the quality of life of persons in the Babylon Valley Stream community through enhanced vision. TRICARE For Life member. CECs portfolio of clients has expanded to a variety of.
Search for the orange Premier banner location nearest to you and get started. At the clinic plan members pay only what their. Vision For Life Corps practice location is.
Youre eligible for TRICARE. Accessible options for eye care. During our almost 30 years of operations we have successfully become the first company in Sri Lanka.
And did we mention WellCard is free. We promote plans with higher exam frequencies we educate our members on their benefits and we provide you with competitive lab solutions. Our experienced eye doctors offer comprehensive vision examinations at our Babylon or Valley Stream optometry office and specialize in the diagnosis and treatment of a wide array of eye diseases conditions and problems.