Michael McLeod MA CCC-SLP is an ASHA-Certified Speech-Language Pathologist. Depending on the treatment she receives and the type of insurance plan her insurance company might say the amount she paid exceeds the allowed amount.
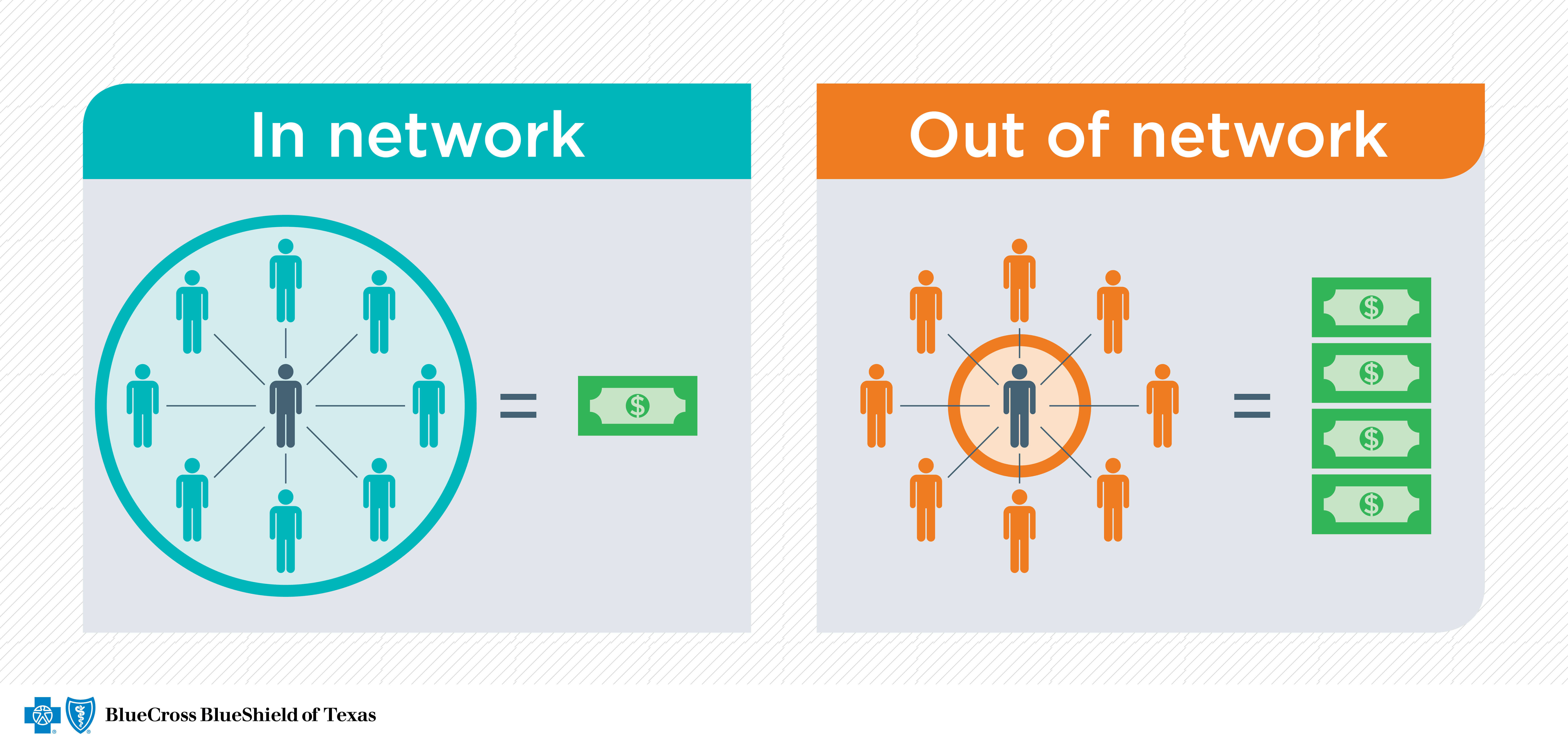 Check Provider Networks Before You Get Care Blue Cross And Blue Shield Of Texas
Check Provider Networks Before You Get Care Blue Cross And Blue Shield Of Texas
Therefore a patient who sees an out-of-network provider can expected to pay much more than if they were to see an in-network provider.
Out of network insurance. GrowNOW Therapy Services LLC is not responsible for out of network service reimbursement. Out of network insurance cost. In or out of network all plans help pay for medically necessary emergency and urgent care services.
Out of network is a health insurance term that refers to health care providers not contracted with the insurer to provide health services at a negotiated rate. Out of network simply means that the doctor or facility providing your care does not have a contract with your health insurance company. Out-of-network means that a doctor or physician does not have a contract with your health insurance plan provider.
Suppose Suzie spends 200 to see a therapist who does not take her health insurance which is a PPO plan she obtains through her employer. How Out-of-Network Reimbursement Works. This means medical providers may charge the full amount for.
Out-of-Network providers can only work with PPO plans excluding rare exceptions. When you get a medical bill if you have health insurance there are two prices. When its not an emergency PPO and HMO plans work differently.
Out of Network Insurance Hunterdon Healthcare is dedicated to providing patients consumers and caregivers with as much information as possible regarding potential health care costs. Delta dental makes it easy for you to get the most value out of your insurance with networks that include more than 155000 dentists nationwide. Provide the client with a superbill and have them file the claim to get reimbursed by their insurance company.
Accordingly we have listed information on the insurers and products we participate in as well as any exceptions. For example if you go to an out-of-network dentist and are billed 300 for the service your insurance company may contribute 200 toward paying this. HMO plans dont include out-of-network benefits.
GrowNOW Therapy Services LLC is a private pay optional service. In-network health care providers have contracted with your insurance company to accept certain negotiated ie discounted rates. This can sometimes result in higher prices.
Some health plans such as an HMO plan will not cover care from out-of-network providers at all except in an emergency. 30 rather than 20. GrowNOW Therapy Services LLC never guarantees.
Before scheduling an appointment or a procedure ask if the provider is in your insurance plans network. Conversely in-network means that your provider has negotiated a contracted rate with your health insurance company. Why does in-network vs out-of-network matter.
We are out of network with all insurances. If a provider is out-of-network this means they are not contracted with your insurance agency. This means that the provider has not signed a contract agreeing to accept the insurers negotiated prices.
So you might be stuck with 30 of a 200 charge 60 plus the 100 difference in doctors fees. You can be charged with out-of-network costs when care is provided and the medical provider has not agreed to a negotiated fee with your insurance provider. This list may not be comprehensive.
Motivating factors for treatment centers to go In-network are predictable reimbursements better communication and authorization periods from the insurance company and access to all HMO and EPO plans. This is the option that most out of network clinicians use because this puts most of the work on the client whether this is good or bad is for your decide. You have two options as an out-of-network provider.
What does out of network mean. Some out-of-network providers choose to avoid contracting with insurance companies altogether and others may only select certain insurances. That means if you go to a provider for non-emergency care who doesnt take your plan you pay all costs.
The amount that a health care insurance plan will contribute toward out-of-network services will vary by your insurance company and is often based on a reasonable and customary amount that the service should cost. This phrase usually refers to physicians hospitals or other healthcare providers who do not participate in an insurers provider network. The coverage your plan offers for in-network and out-of-network.
Because out-of-network costs add up quickly it is important you become familiar with your plan and whether your health care provider is in your network. Plus you may be responsible for the difference between the in-network and out-of-network bills 100. For the out-of-network doctor your insurance company might charge you a higher coinsurance percentage eg.
Health insurance companies would prefer you to seek care from their in-network providers because it costs them.
 Understanding The Difference Between In Network And Out Of Network Provider Coverage
Understanding The Difference Between In Network And Out Of Network Provider Coverage
3 Things To Consider When Signing Up For Health Insurance
 Using Out Of Network Doctors Could Cost You Money Ehealth
Using Out Of Network Doctors Could Cost You Money Ehealth
Out Of Network Benefits Doctor K Private Medicine
 In Network Or Out Of Network What S The Difference
In Network Or Out Of Network What S The Difference
 In Network And Out Of Network Dentist Which Is Better
In Network And Out Of Network Dentist Which Is Better
Does Out Of Network Care Really Cost More Than In Network Care
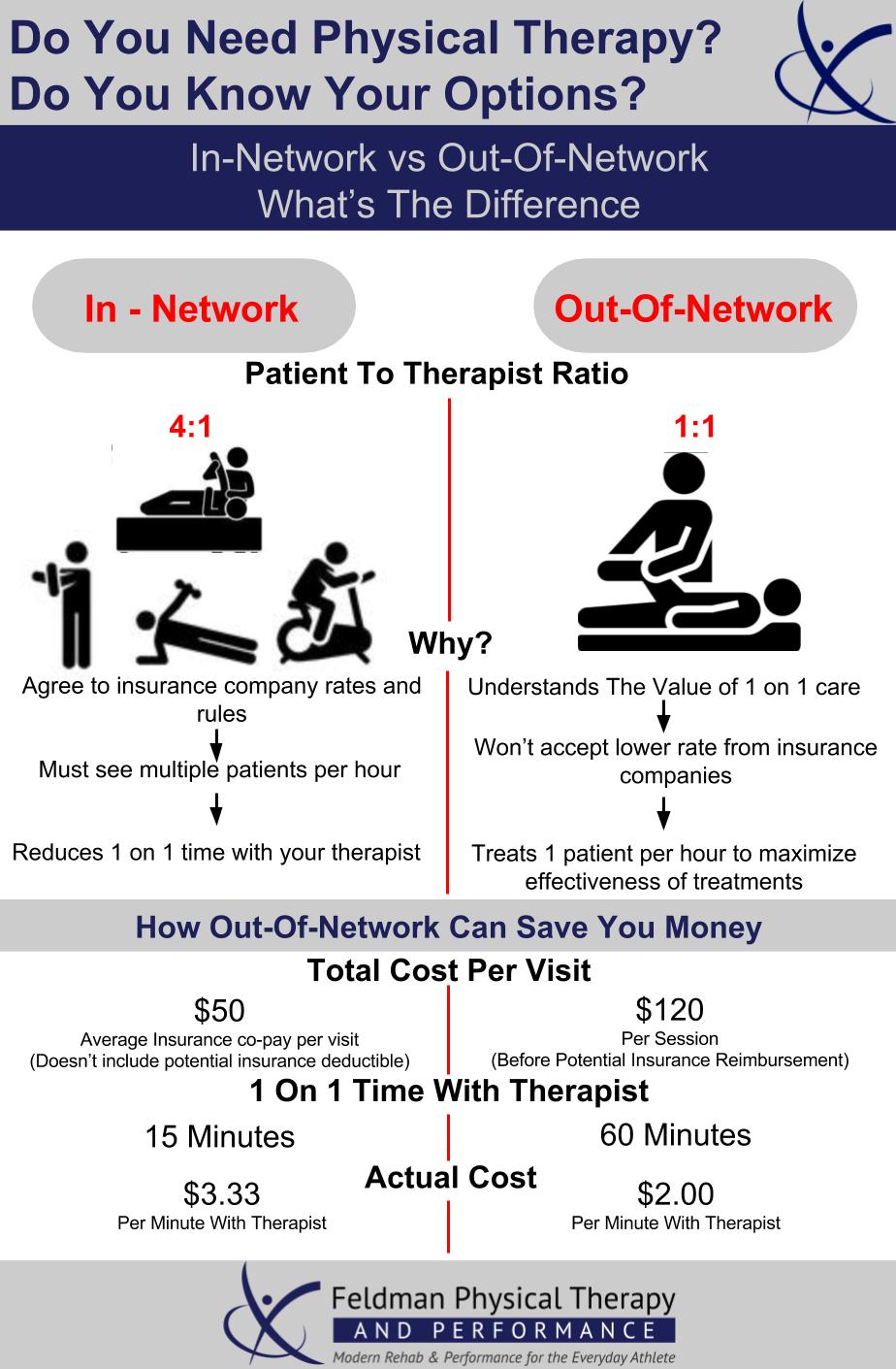
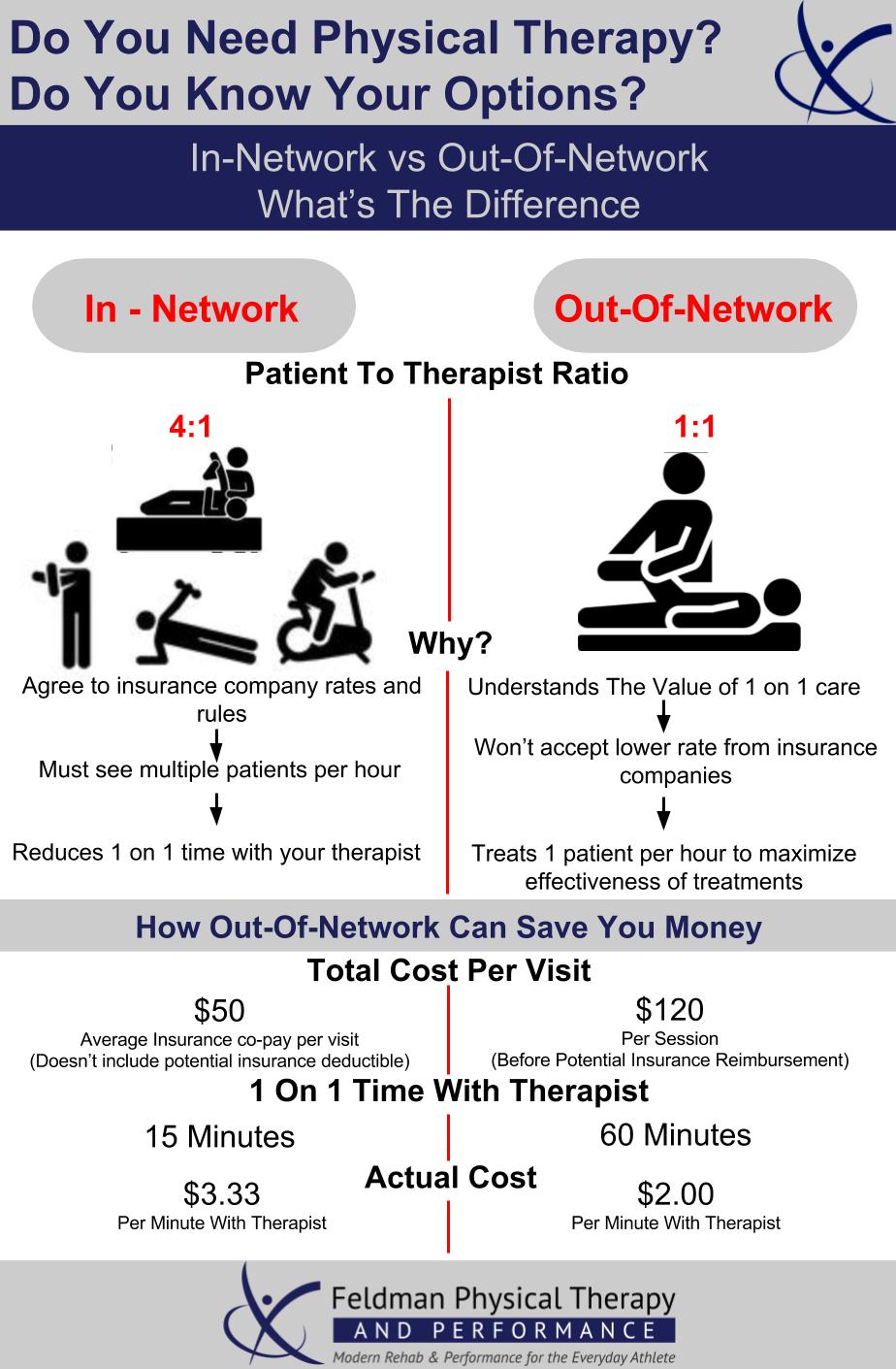 Why We Choose To Be An Out Of Network Provider Feldman Physical Therapy And Performance
Why We Choose To Be An Out Of Network Provider Feldman Physical Therapy And Performance
 How Often Do Providers Bill Out Of Network Hcci
How Often Do Providers Bill Out Of Network Hcci
 Does My Doctor Know What Providers Are In My Network Nh Health Cost
Does My Doctor Know What Providers Are In My Network Nh Health Cost
In Network Vs Out Of Network Care Katz Insurance Group
 What Are Provider Networks Nh Health Cost
What Are Provider Networks Nh Health Cost
 Out Of Network Dentist Myths Debunked Chester Mendham Dental
Out Of Network Dentist Myths Debunked Chester Mendham Dental


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.