Anthem Blue Cross Anthem is available by fax or Interactive Care Reviewer ICR 247 to accept prior authorization requests. Non-Formulary Exception and Quantity Limit Exception PDF 129 KB Prior AuthorizationCoverage Determination Form PDF 136 KB Prior Authorization Generic Fax Form PDF 173 KB.
 Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
Anthem Blue Cross Blue Shield Prior Prescription Rx Authorization Form Authorization Forms
If the provider or member doesnt get prior authorization for out-of-network services the claim may be denied.
Blue cross prior authorization form. FEP will waive prior authorizations for medically necessary diagnostic tests and covered services that are consistent with CDC guidance if diagnosed with. A Mutual Legal Reserve Company an Independent Licensee of the Blue Cross and Blue Shield Association. Please allow 24 to 48 hours after we receive all the information for a response.
You are leaving our website and going to a websiteapp not hosted by us. Request form instructions Providers. Emergency services are an exception.
Our Interactive Care Reviewer ICR tool via Availity is the preferred method for submitting prior authorization requests offering a streamlined and efficient experience for providers requesting inpatient and outpatient medical or behavioral health services for our. For Medical Policy information please visit our website at. However where appropriate the content may identify a particular company.
Submit by fax using the forms posted on the FutureScripts website. Information for Blue Cross and Blue Shield of Illinois BCBSIL members is found on our member site. Requests will be confidentially reviewed according to payment criteria developed by Blue Cross in consultation with independent health care consultants.
Prior Authorization Requests Prior Authorization is a pre-approval process to determine if certain prescription drugs will be reimbursed under a members benefit plan. Weve provided the following resources to help you understand Empires prior authorization process and obtain authorization. Fill out a transition of care form.
To request prior authorization for these medications please submit the. The forms in this online library are updated frequentlycheck often to ensure you are using the most current versionsSome of these documents are available as PDF files. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required.
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan. Fax Number Phone Number 1-888-260-9836 1-888-261-1756. Generally the pronouns our we and us used throughout this website are intended to refer collectively to Blue Cross and Blue Shield of Florida Inc.
Blue Cross Blue Shield of Michigan Request for Preauthorization Form. Please fax this back to Pharmacy Services. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
And its subsidiaries and affiliates. To find a prior authorization form visit our forms. This is called a prior authorization.
Prior authorization requests are reviewed by FutureScripts our independent pharmacy benefits manager on behalf of Independence. A library of the forms most frequently used by health care professionals. If you do not have Adobe Reader download it free of charge at Adobes site.
Massachusetts Collaborative Massachusetts Standard Form for Medication Prior Authorization Requests May 2016 version 10 MASSACHUSETTS STANDARD FORM FOR MEDICATION PRIOR. Pharmacy Services Prior AuthorizationRequest Form. Most out-of-network services require utilization management review.
Premera Blue Cross Blue Shield of Alaska is an Independent Licensee of the Blue Cross Blue Shield Association serving businesses and residents of Alaska and. Learn more about submitting prior. Member authorization is embedded in the form for providers submitting on a members behalf section C.
Massachusetts Standard Form for Medication Prior Authorization Requests eForm or contact Clinical Pharmacy Operations. However if you would like to submit a request for preauthorization after contacting PRS you may submit a written request by completing this form. Blue Shield of California Promise Health Plan Medi-Cal and Cal MediConnect.
Find authorization and referral forms. Most preauthorization requests can be resolved by contacting Provider Relations and Servicing or PRS and requesting member benefits. Blue Choice members using their self-referred benefit do not need to get prior authorization.
Independent licensees of. Prior Authorization Lookup Tool. There any pronouns refer to.
A request form must be completed for all medications that require prior authorization. Submit a prior authorization Reviewed by BlueCross BlueShield. The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost.
Anthem Blue Cross is the trade name of Blue Cross of California and Anthem Blue Cross Partnership Plan is the trade name of Blue Cross of California Partnership Plan Inc. Prior authorization and pre-approval. Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification.
Blue Cross Blue Shield of Massachusetts Health Plan Phone. Requests for the following services can be made by fax or mail.
 Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
Free Anthem Blue Cross Blue Shield Prior Rx Authorization Form Pdf Eforms
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
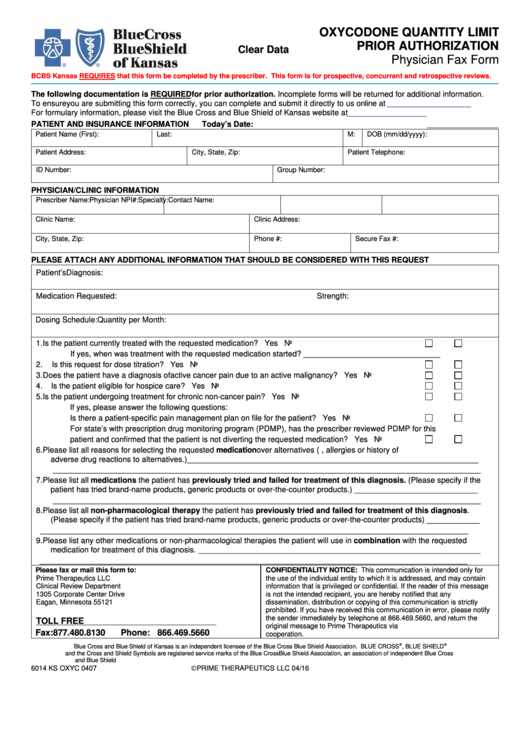
 Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
Free Prime Therapeutics Prior Rx Authorization Form Pdf Eforms
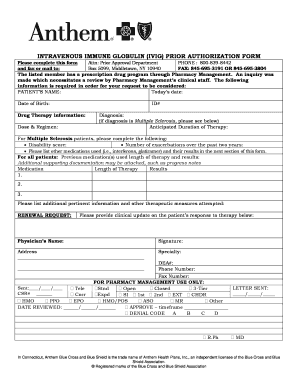
Https Www Anthem Com Provider Noapplication F0 S0 T0 Pw E228625 Pdf Na Pharminfo
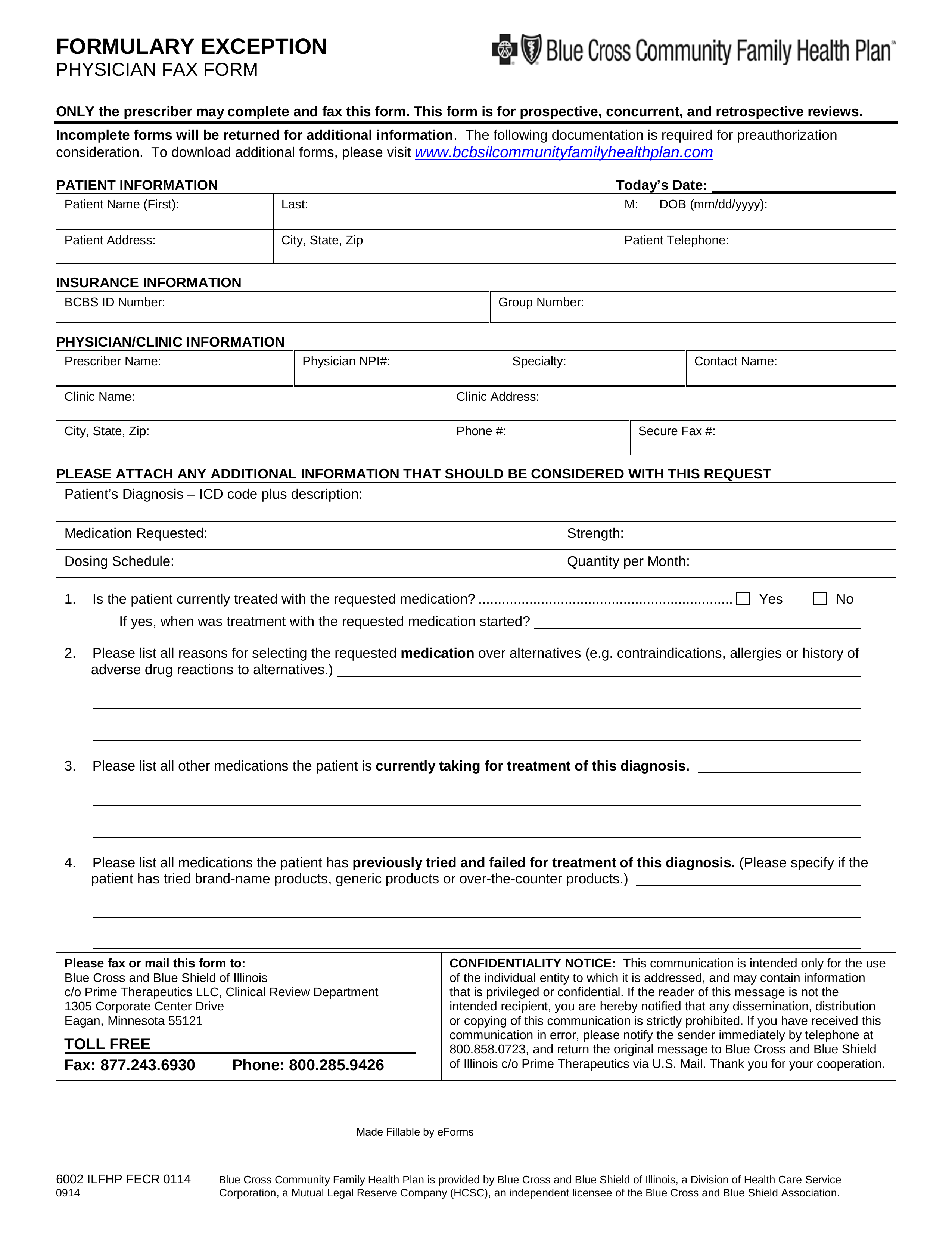
Https Www Bcbsil Com Pdf Education Forms Fhp Preauth Form Pdf
Https Www Blueshieldca Com Bsca Bsc Public Common Portalcomponents Provider Streamdocumentservlet Filename Prv Fep Medical Injectable Drug Pdf
 Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Anthem Prior Authorization Form Pdf Fill Online Printable Fillable Blank Pdffiller
Https Bluecrossnc Com Sites Default Files Document Attachment Common Pdfs Hmo Ppo General Quantity Limitations Fax Request Form Pdf
Https Www Azblue Com Media Azblue Files Pharmacy Forms Mastery Directory Standard Pharmacy Plans Other Forms And Resources Pharmacy Prior Authorization Request Form Pdf
 Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Bcbs Of Massachusetts Medication Prior Authorization Form Beautiful Blue Cross Blue Shield Massachusetts Prior Authorization Form Models Form Ideas
Https Providers Bcbsal Org Portal Documents 10226 301829 General Prescription Drug Coverage Authorization Request Form A9b9b8bf 922b 469a B21f E396da68c634 Version 1 5
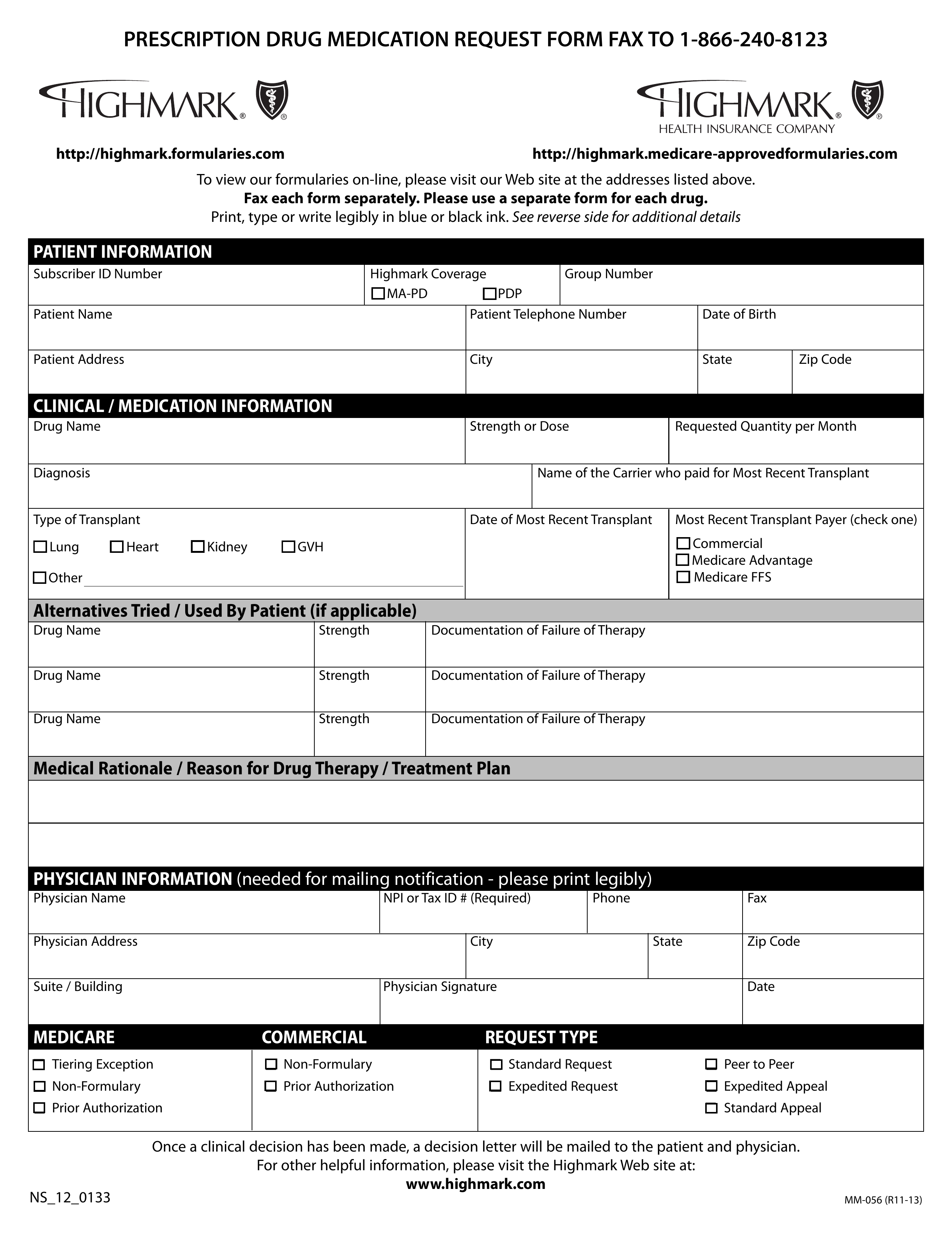 Free Highmark Prior Rx Authorization Form Pdf Eforms
Free Highmark Prior Rx Authorization Form Pdf Eforms
Https Www Empireblue Com Provider Noapplication F3 S2 T2 Pw Ad067834 Pdf Refer Ehpprovider
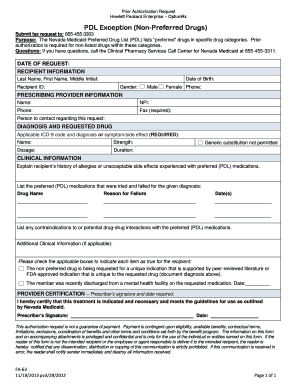 2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller
2012 Form Nv Fa 63 Fill Online Printable Fillable Blank Pdffiller

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.