If you come to see us and you are In-Network if there is a difference in the fee for any particular service between what OUR fee is and what your insurance ALLOWS for that service ie. How does out-of-network coverage work.
 How Do Commerical Ppo Vs Hmo Insurance Plans Work Dr Wenjay Sung Podiatrist
How Do Commerical Ppo Vs Hmo Insurance Plans Work Dr Wenjay Sung Podiatrist
This means that most insurance plans allowing members to go out-of-network for mental health will reimburse you for our work according to the payments they allow.
How does out of network insurance work. Some health plans such as an HMO plan will not cover care from out-of-network providers at all except in an emergency. In Network Versus Out of Network Coverage. For cosmetic or complex dental treatments it is better to choose a dentist that will suit your needs and who has.
What does out-of-network mean. If the client would pay you your full fee as an out-of-network provider you would indicate this on your claim form and select NO in boxes 13 and 27 so that the insurance company reimburses the client. Conversely in-network means that your provider has negotiated a contracted rate with your health insurance company.
HOW DO OUT-OF-NETWORK DENTISTS WORK. Out of network simply means that the doctor or facility providing your care does not have a contract with your health insurance company. This example demonstrates how quickly health care costs can add up for services provided by out-of-network professionals.
And its important to understand that out-of-network providers can and do balance bill patients for the remainder of the charges after the insurance company has paid its share. They help pay for care you get from providers who dont take your plan. You avoid running the risk of getting low-quality dental treatments just because you have to choose a dentist from the.
UCRs are fee guidelines that rein in the amount providers can charge for out-of-network patients and serve as a guideline insurers use to determine the amount they will pay for out-of network care. Out-of-network refers to a health care provider who does not have a contract with your health insurance plan. But you usually pay more of the cost.
In Network Vs Out Of Network Out Of Pocket Maximum. As with the deductible the out of pocket maximum could be different for in network coverage or out of network coverage. In-network providers have agreed to accept the insurance companys payment plus the patients pre-determined cost-sharing amount as payment in full but out-of-network providers have not.
Out of network your plan may 60 percent and you pay 40 percent. Learn more about the differences between in- and out-of-network health benefits. Allowable Fee then we Write-Off the difference.
This can sometimes result in higher prices. For Preventive and Diagnostic services covered. Because out-of-network costs add up quickly it is important you become familiar with your plan and whether your health care provider is in your network.
If you reach your out of pocket maximum the insurance company will pay 100 of covered services. Insurance policies usually have an out of pocket maximum value that limits how much a person will pay out of pocket total annually. PPO plans include out-of-network benefits.
Insurance pays 50 of the remaining allowables which would work out to 5000 2 2500 and you would owe the other 2500 which would of course go toward your out of network out. The amount that a health care insurance plan will contribute toward out-of-network services will vary by your insurance company and is often based on a reasonable and customary amount that the service should cost. Our licenses training and education qualify for out-of-network reimbursement.
If you use an out-of-network provider health care services could cost more since the provider doesnt have a pre-negotiated rate with your health plan. Health insurance companies would prefer you to seek care from their in-network providers because it costs them less. When you are out-of-network you have the option of sending the payment to the clinician or to the client.
To keep costs under control ask providers if they are contracted with your insurance plan. If you choose to see an out-of-network. For example your plan may pay 80 percent and you pay 20 percent if you go to an in-network doctor.
Out-of-network means that a doctor or physician does not have a contract with your health insurance plan provider. You can still use your. You can be charged with out-of-network costs when care is provided and the medical provider has not agreed to a negotiated fee with your insurance provider.
For example my in network out of pocket maximum is 6700 but my out of network. Check the nature of your insurance and what it will reimburse you.
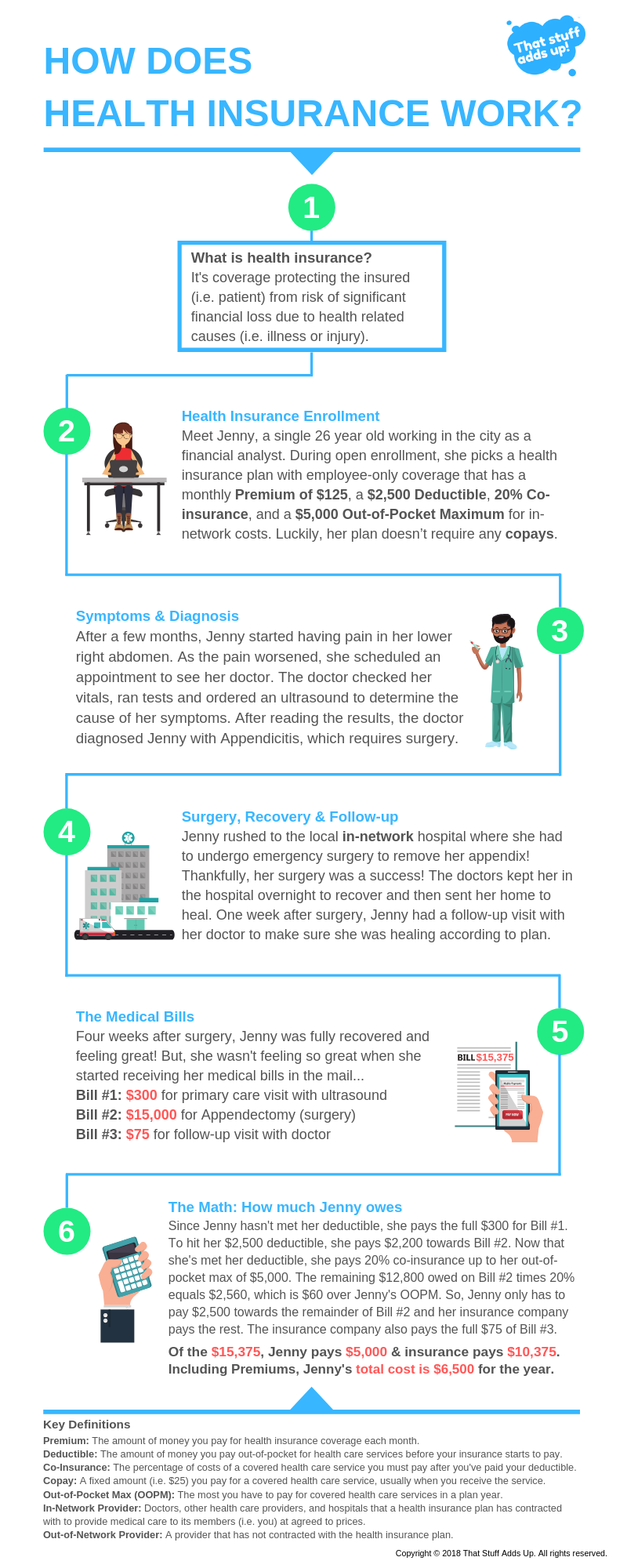
 How Health Insurance Works That Stuff Adds Up
How Health Insurance Works That Stuff Adds Up
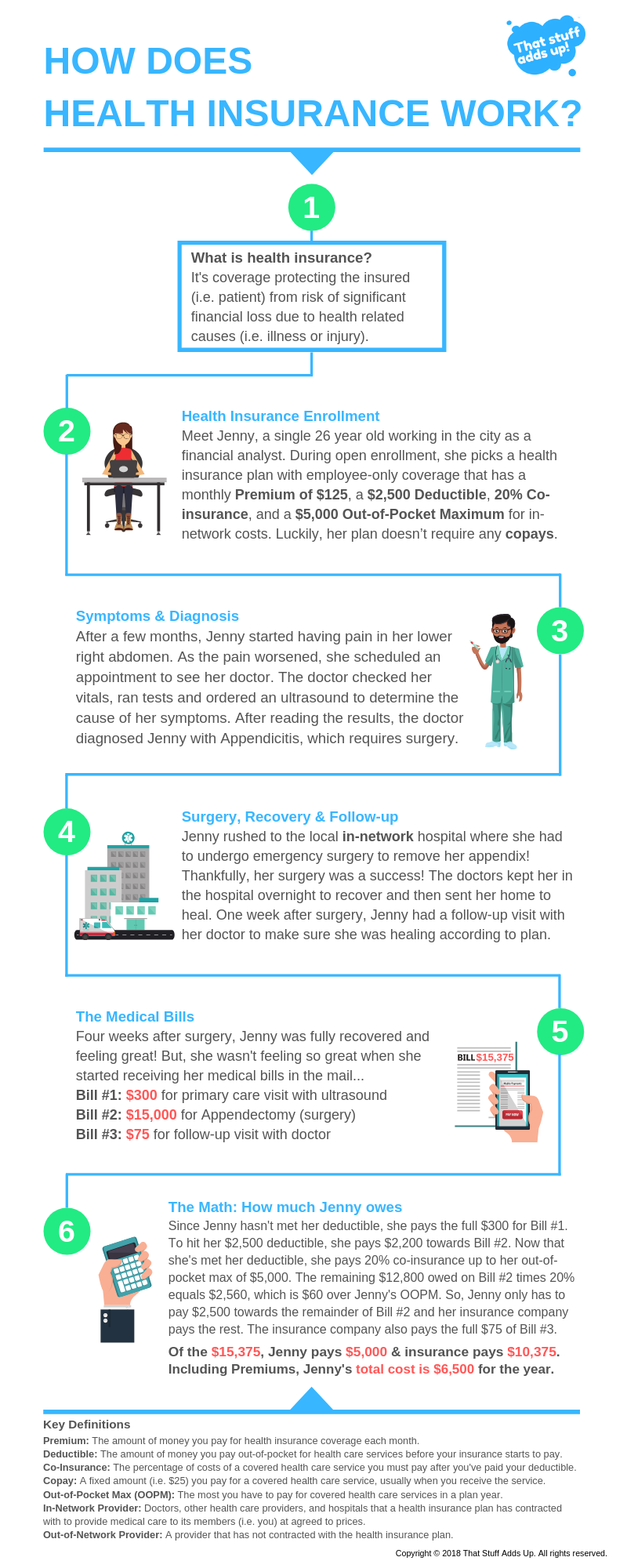
 Check Provider Networks Before You Get Care Blue Cross And Blue Shield Of Texas
Check Provider Networks Before You Get Care Blue Cross And Blue Shield Of Texas
/Health-insurance-5687e75d5f9b586a9e4dd055.jpg) Dealing With Out Of Network Healthcare Bills
Dealing With Out Of Network Healthcare Bills
 In Network And Out Of Network Dentist Which Is Better
In Network And Out Of Network Dentist Which Is Better
 In Network Vs Out Of Network What Does Out Of Network Mean
In Network Vs Out Of Network What Does Out Of Network Mean
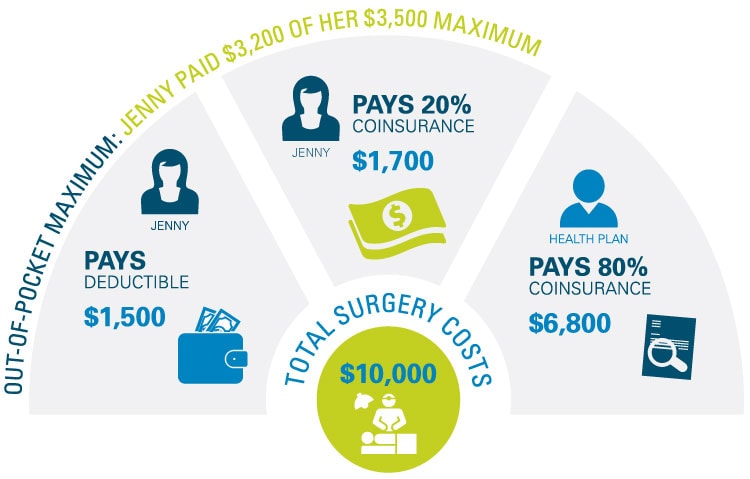 What Is An Out Of Pocket Maximum Bluecrossmn
What Is An Out Of Pocket Maximum Bluecrossmn
3 Things To Consider When Signing Up For Health Insurance
 Understanding The Difference Between In Network And Out Of Network Provider Coverage
Understanding The Difference Between In Network And Out Of Network Provider Coverage
 Saving Money On Therapy With Out Of Network Insurance Benefits
Saving Money On Therapy With Out Of Network Insurance Benefits
 What Type Of Health Plan Works Best For Me Choosing The Right Plan Independence Blue Cross
What Type Of Health Plan Works Best For Me Choosing The Right Plan Independence Blue Cross

/health-insurance-card-56a695705f9b58b7d0e3b3ca.jpg) What An Out Of Network Provider Means
What An Out Of Network Provider Means
 In Network And Out Of Network Dentist Which Is Better
In Network And Out Of Network Dentist Which Is Better


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.