2 of 3 Wen Liu the pharmacist at the Walgreens on powell fills prescriptions. If your pharmacy is an in-network provider and is encountering any issues with Medi-Cal MCP or FFS reimbursement of vaccines contact the respective health plan or Medi-Cal Provider Helpline at 1-800-541-5555.
 Iris Dedicated Solutions For Drugstores Pharmacies
Iris Dedicated Solutions For Drugstores Pharmacies
Improve Medi-Cal beneficiary access to pharmacy services with a pharmacy network that includes approximately 94 of the states pharmacies.

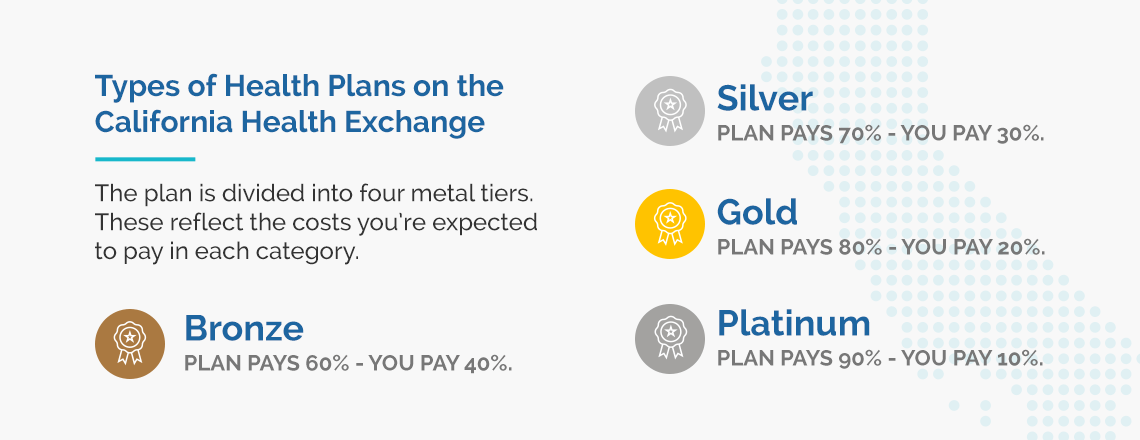
What pharmacies accept medi cal. Welcome to the Medi-Cal Provider Home. Your choices will depend on the county you live in. Under the Final Rule each state Medicaid agency was required to adopt an actual acquisition cost AAC based methodology for CODs.
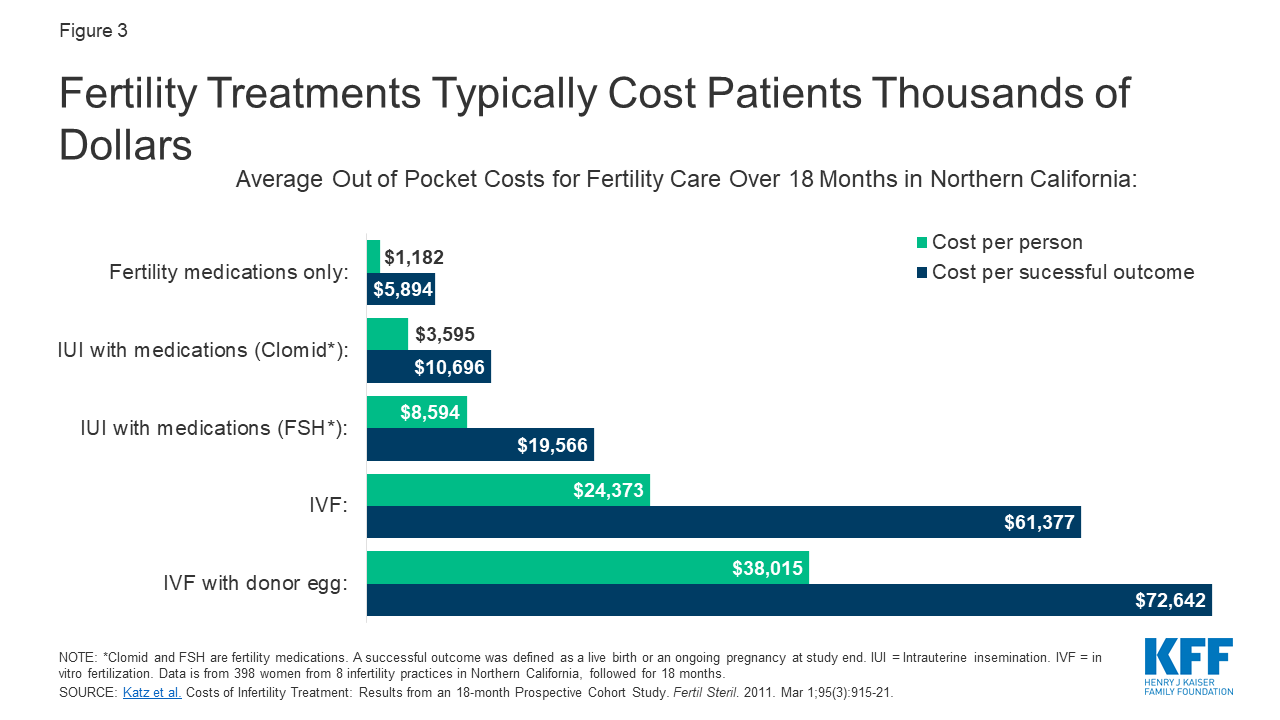
Walgreens which has 360 pharmacies in the state is threatening to stop filling Medi-cal prescriptions because of the. July Online Training Sessions Being Offered for Providers. You may also contact us at PPNOhealthnygov or 518 486-3209 for Medicaid pharmacy policy related questions.
For more information and copies of letters sent to pharmacists and prescribers please see Pharmacy Provider Communications below. Please check the formularies listed below to see if a medication requires prior authorization. Temporary Increased COVID-19 Freestanding Skilled Nursing Facility Level B Rates.
The Centers for Medicare Medicaid Services CMS published its Final Rule for Covered Outpatient Drugs CMS-2345-FC on February 1 2016. Under the guidance of the California Department of Health Care Services the Medi-Cal fee-for-service program aims to provide health care services to about 13 million Medi-Cal beneficiaries. With the MeridianRx Mobile App you can access your pharmacy benefits quickly and easily.
Medi-Cal Rates are updated and effective as of the 15th of the month and published to the Medi-Cal website on the 16th of the month. CCS Service Code Groupings Update for COVID-19 Services. Prior authorization forms are appropriate for both Commercial and Medicaid lines and must be completed by the prescribing physician.
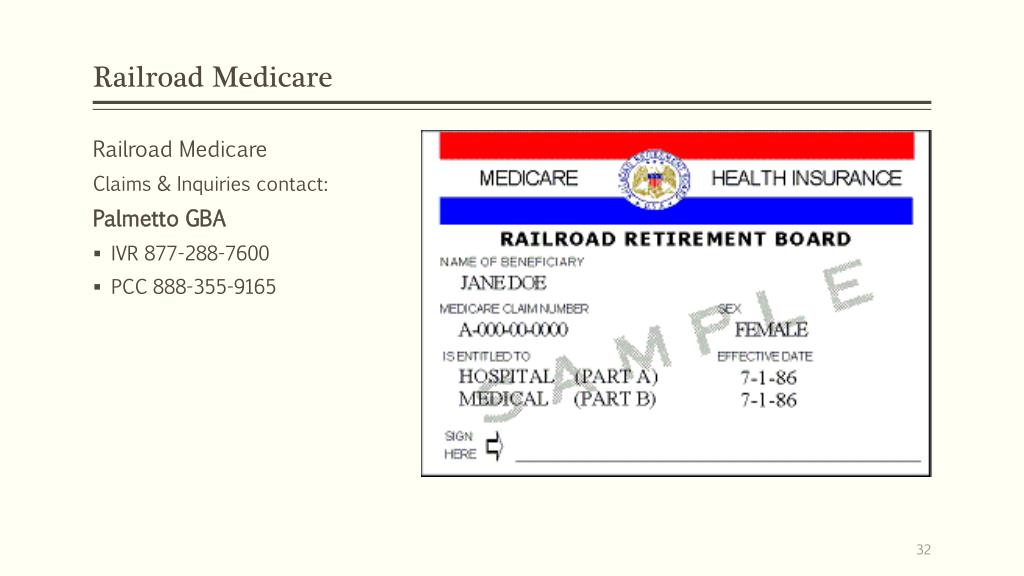
Access automated provider services for claims eligibility inquiry and other Medi-Cal services New Provider Welcome new providers access content to. Providers must contact the individual Medi-Cal Health. 247 Free Medi-Nurse Call Line Launches for COVID-19 Questions.
NHS Volunteer Responders can help with collecting medicines and prescriptions. Effective for dates of service on or after March 1 2009 Medi-Cal payments to providers unless exempted will be subject to a 1 or 5 reduction based on provider type. The following information may be of interest to pharmacists and prescribers.
Medi-Cal Pharmacy Provider Self-Attestation Period Now Open. Using Your Medi-Cal Coverage. Search the MeridianRx pharmacy network by name location and coverage type.
You can also pay for the prescription but still request a TAR be sent. Find a Physician Who Accept Medi-Cal in California. To satisfy this requirement California along with many other state Medicaid.
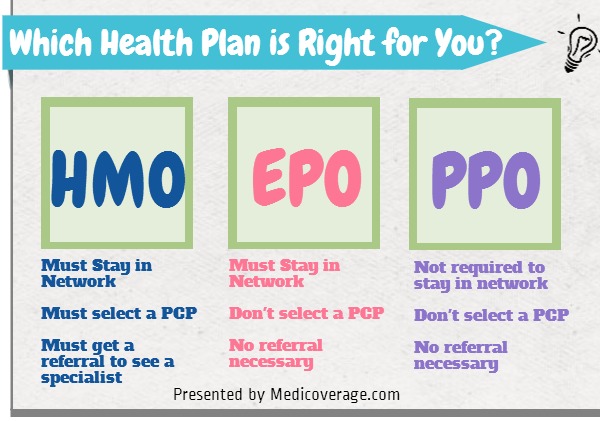
If you do not choose a health plan within 30 days Medi-Cal will choose a plan for you. Family PACT Retroactive Enrollments for Eligibility Transactions. Elixir pharmacy staff are available 24 hours a day at 1-844-222-5584 Prior Authorizations.
Download our members-only mobile app to. You may be able to get your medicines delivered you may have to pay for this or ask someone to collect them. You live with someone who has symptoms.
Get turn-by-turn directions to a nearby network pharmacy. Most insurance plans have online member assistance and many companies also allow you to call them to receive direct help. Limits Removed from ICD-10-CM Code U071 for Aid Code V2.
Each Medi-Cal Health Plan is unique in its billing and service procedures. Call 0808 196 3646 8am to 8pm every day to arrange help from a volunteer. Getting your prescriptions filled is as easy as looking up a participating pharmacy near you and presenting your EmblemHealth ID card.
Medi-Cal Rates as of 12152020. Other changes resulting from the transition to FFS include. Medi-Cal Rx Subscription Service and Pharmacy Service Representative Phone Campaign.
Beneficiaries enrolled in Medi-Cal Health Plans must receive Medi-Cal pharmacy benefits from plan providers. If the medicine is something you need immediately you can request enough medicine for 72-hours from your pharmacist while you wait for approval from Medi-Cal. Medi-Cal Health Plans are required to provide or arrange for medically necessary outpatient pharmacy services.
These Medi-Cal pharmacy benefits and services administered by DHCS in the FFS delivery system will be identified collectively as Medi-Cal Rx. When you qualify for Medi-Cal you will receive a packet in the mail with health plans you can choose from. Medi-Cal members can receive member services through the Internet or by phone.
If the medication is approved after the fact the pharmacy is required to refund your money. New pharmacy regulations require that pharmacists. The Medi-Cal fee-for-service program adjudicates both Medi-Cal and associated health care program claims.
Our Individual Qualified Health Plans Essential Plans and Small Group Plans no longer offer CVS and Target as in-network pharmacy locations. Contact a MeridianRx pharmacy MeridianHealth or PCP. Covered California also has online member services that you can access through an account.
Find a Physician Who Accept Medi-Cal in.