High technology diagnostic imaging requests for CTMRIPET examinations that are related to immediate care of a medical emergency or associated with an inpatient hospital admission do not require prior approval. They said they will not cover it because of pre-existing.
Https Provider Bluecrossma Com Providerhome Wcm Connect 616ea312 E3cd 4759 9a02 90f8a506f2a5 Fep Um Guideline 003 Outpatient Htr Pdf Mod Ajperes
If you do not get approval from Blue Cross and Blue Shield of Vermont before administration benefits may be reduced or denied.
Blue cross blue shield mri approval. Outside the United States. If you need preapproval your doctor or health care professional will request a review on your behalf. Diagnostic imaging requests for CT MRI and PET examinations.
One of the most important steps is prior authorization. Online Prior Approval Management Blue Cross Blue Shield of Vermont Online Prior Approval Management Use these online tools to submit and check the status of prior approval requests for BCBSVT members. In the United States Puerto Rico and US.
Advanced Radiology Imaging PreauthorizationPrenotification Requirements Through eviCore for Blue Choice PPO With Health Advocacy Solutions Members March 2 2018 On Oct. Services that need approval. Your cost on paper after applying Blue Cross Blue Shield will likely be somewhere between your deductible and that.
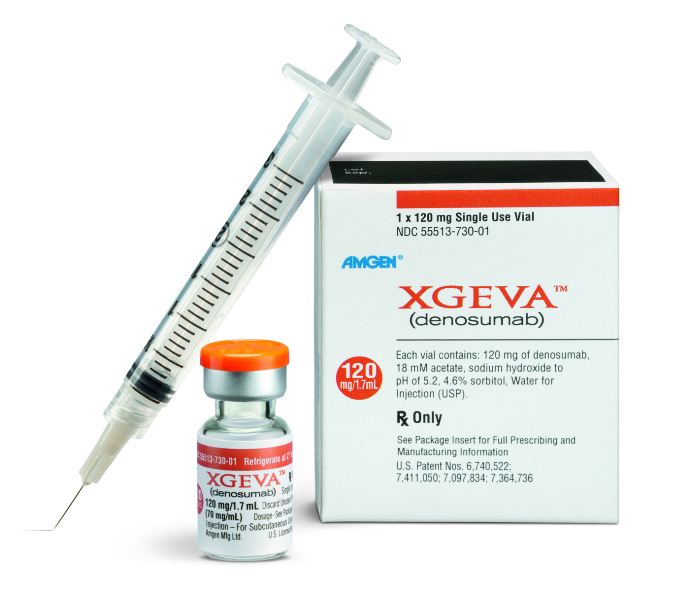
Your doctor prescribes it in a medically appropriate way You can see the full list of prescription drugs that need to be approved on the CVS Caremark website. In the meantime Morgan decided he would rather have the scan at Penn where he had already been examined and. Any device utilized for this procedure must have FDA approval specific to the indication otherwise its use will be considered investigational.
MEDICAL APPROPRIATENESS Magnetic Resonance Imaging MRI of the breast is considered medically appropriate if ANY ONE of the following are met. In California That MRI Will Cost You 255 Or Maybe 6221 NPR How Hospitals Determine the Price of an MRIand Why Clinics Can Charge Less -. Once we get the request well begin the review process.
Available Monday through Friday 8 am. Blue Cross Blue Shield members can search for doctors hospitals and dentists. Only ordering physicians can obtain a prior plan approval number.
Prior review prior plan approval prior authorization prospective review or certification is the process Blue Cross NC uses to review the provision of certain behavioral health medical services and medications against health care management guidelines prior to the services being provided. Vincera submitted the MRI to Blue Cross for prior authorization and it was approved Aug. 15081 satisfied customers Blue Cross and Blue Shield Insurance Company gave approval Blue Cross and Blue Shield Insurance Company gave approval for MRIover 20 years ago.
Prior approval - Arkansas Blue Cross and Blue Shield Prior approval program information High-tech imaging scanning procedures are one of the most rapidly rising medical expenses. Most are exposing patients to. Blue Cross Blue Shield of RI BCBSRI Radiology Management program vendor for BlueCHiP for Medicare and Commercial Products.
Forms and additional information can be downloaded on the CVS Caremark website. Your doctor can submit prior approval electronically by fax or by mail. MEDICAL CRITERIA BlueCHiP for Medicare and Commercial Products Clinical guidelines for approval of the tests listed below are found on the Radiology Management Program vendors website.
Servicing providers hospitals freestanding imaging centers etc should confirm that a prior approval number has been issued. Approval information for radiological services An outpatient diagnostic imaging program is active since September 1 2006 for individual and group members of Arkansas Blue Cross and Blue Shield health plans except for members of Medi-Pak Medi-Pak Advantage Access Only AR Health where Medicare is primary BlueCard check with home plan if not Arkansas and the Federal Employee Program FEP. Prior ApprovalAuthorizations - Requirements Forms.
Call AIMs Contact Center at 1-866-745-1783. If youve already registered for the AIM ProviderPortal for Blue Cross Blue Shield of Massachusetts or another insurer you wont need to register again. If you leave a voicemail after these hours AIM will respond the next business day.
A Effective November 22 1985. MRI is useful in examining the head central nervous system and spine. We call this prior authorization.
Many times your doctor will need to get approval prior authorization before your plan will cover certain health care services and medicines. The following high-tech scans are not only causing premiums to increase. Select Blue Cross Blue Shield Global or GeoBlue if you have international coverage and need to find care outside the United States.
Depending on what type of plan you have we may need to review and approve some of your health care services before we cover them. FDA premarket approval and such units must be operated within the parameters specified by the approval. In addition the services must be reasonable and necessary for the diagnosis or treatment of the specific patient involved.
2 2017 Blue Cross and Blue Shield of Texas BCBSTX posted a notice regarding benefit preauthorization requirements for Blue Choice PPO members with health advocacy solutions in the Disclosures. 15 according to a letter Morgan received from Blue Cross. Ordering physicians for Blue Cross NC members must obtain prior approval prior to scheduling an imaging exam for outpatient diagnostic non-emergent services.
Prior Approval List of services drugs and supplies that require approval from Blue Cross and Blue Shield of Vermont prior to administration andor admission. Your doctor may also call it preauthorization and preapproval.