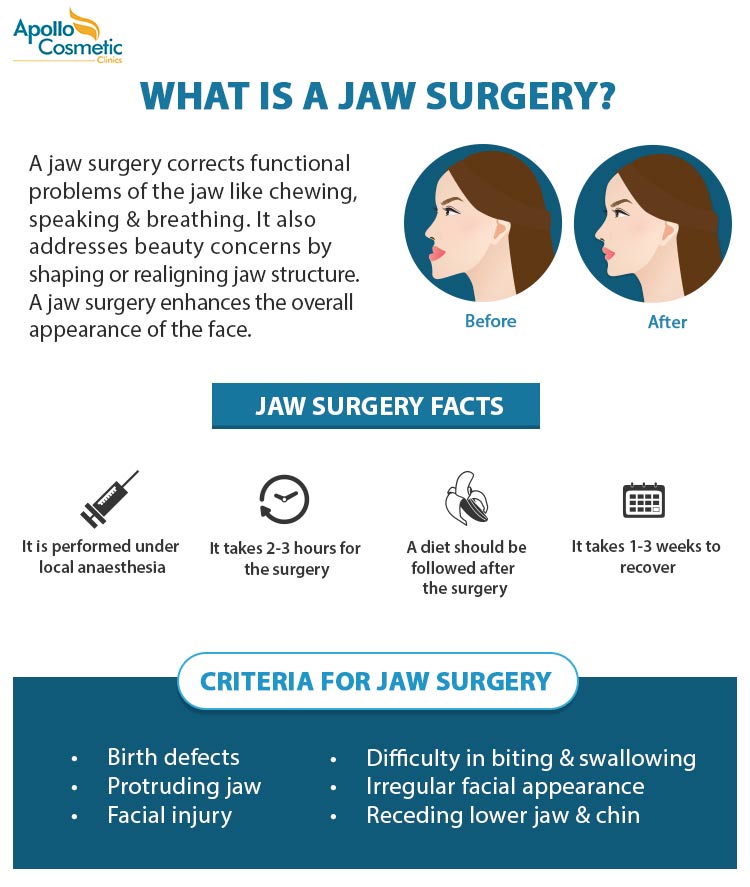
Will Regence Blue Cross or Kaiser cover this. However many health insurance policies cover orthognathic corrective jaw surgery and getting insurance coverage for jaw surgery is easier than many people might think.
 Jaw Surgery In Chennai Orthognathic Surgery Apollo Cosmetic Clinics
Jaw Surgery In Chennai Orthognathic Surgery Apollo Cosmetic Clinics
Effective May 1 2019 Horizon BCBSNJ will change the way we consider certain professional claims based on revisions to our medical policy Orthognathic Surgery.

Orthognathic surgery insurance blue cross. DESCRIPTION OF PROCEDURE OR SERVICE Orthognathic surgery is a class of surgical procedures designed to realign the maxillofacial skeletal structures with each other and with the other craniofacial structures. Does it go through dental or health insurance. The following represents exceptions to the orthognathic jaw surgery exclusoi n and may be eligible for coverage as reconstructvie and medicayll necessary.
Claims submitted for services provided on and after May 1 2019 to patients enrolled in Horizon BCBSNJ commercial. Description Orthognathic surgery is covered when provided by a participating provider notified in advance and meets Blue Cross Completes clinical guideline. These abnormalities may be recognized at birth or may not become obvious until the individual grows and develops.
This study assessed the validity of the medical insurance guidelines for orthognathic surgery used by Aetna Anthem Blue Cross Blue Shield BCBS Cigna Humana and UnitedHealthcare UHC. Orthognathic surgery is performed to correct malocclusion which cannot be improved with routine orthodontic therapy and where the functional impairments are directly caused by the malocclusion. If your surgeon was in-network then you are not responsible for anything over that 5000.
Though orthognathic surgery might be necessary to improve your bite make sure you protect yourself financially before having the surgery. I really want this surgery but I cant afford 20000. This is where patients get in to a lot of trouble.
Materials and Methods This study assessed the validity of the medical insurance guidelines for orthognathic surgery used by Aetna Anthem Blue Cross Blue Shield BCBS Cigna Humana and UnitedHealthcare UHC. An Independent Licensee of the Blue Cross and Blue Shield Association Orthognathic Surgery c Treatment with orthodontic andor splint therapy Note. Receipt of benefits is subject to satisfaction of all terms and conditions of the coverage.
Orthognathic surgery is not covered for BlueCHiP for Medicare members as CMS considers these procedures to be dental and dental services are not covered. Grant McGann works very hard to make sure that his patients insurance policies cover their jaw. To evaluate the validity we calculated the approval and denial rates of the 5 guidelines when we used them to assess the medical necessity for a control group of carefully.
Orthognathic Surgery Insurance QA. He said my insurance stated that they would only cover the surgery for people with cancer sleep apnea or those who had been in a car accident. He said there was nothing he could do and that even if I had orthodontic work done it would likely relapse and be a waste.
Members and members of any third-party Medicare plans supported by Blue Cross NC through administrative or operational services. Thu Nov 12 2015 524 am. There are currently 83 Orthognathic Surgery Insurance questions and doctor answers on RealSelf.
The underlying abnormality may be congenital intrinsic present at birth. Usually somewhere between 50-70 of the allowable amount. In many cases orthodontic treatment alone cannot correct the abnormality.
This policy identifies when corrective jaw surgery. ORTHOGNATHIC SURGERY INSURANCE QUESTIONS. If you dont have insurance either work out a payment plan in advance or plan the surgery after securing the necessary insurance.
Then you can truly enjoy your enhanced quality of life. When it has been determined in advance by cephalometrics and clinical examination that no amount of orthodontic. Anthem BCBS and Orthognathic Surgery.
Acute traumatic in jury Cancerous or non -cancerous tumors and cysts. This study assessed the validity of the orthognathic surgery guidelines used by Aetna Anthem Blue Cross Blue Shield BCBS Cigna Humana and UnitedHealthcare UHC. Examples of conditions for which this surgery is used are mandibular prognathism crossbite open bite overbite underbite mandibular deformity and maxillary deformity.
Anthem BCBS is a merger of a bunch of insurance companies. Orthognathic surgery is the surgical correction of skeletal abnormalities of the mandible maxilla or both. Considering Id spend 2 nights in the hospital maybe both.
My teeth are getting ruined. Orthognathic surgery treats and corrects problems with the facial bones specifically the upper jaw maxilla and lower jaw mandible. Your surgeon can bill a 10000 surgery but your plan has a reasonable and customary allowable amount of 5000.
They have consistent coverage criteria across the board although the actual policies vary widely by state employer etc. Our medical policies are designed for informational purposes only and are not an authorization explanation of benefits or a contract. To evaluate the validity we calculated the approval and denial rates of the 5 guidelines when we used them to assess the medical necessity for a control group of carefully.
MP 701501 - Orthognathic Surgery. Orthognathic surgery is considered medically necessary when the severity of the skeletal deformity results in. Orthognathic jaw surgery is a standard exclusoi n from coverage in most fully -insured plans.
They are based in Indianapolis. Access our Medical Policy Manual to review this medical policy content¹. More about Orthognathic Surgery.
Some of these corrective surgeries involve lengthening or shortening the lower jawbone. At McGann Facial Design San Diego oral and maxillofacial surgeon Dr. Blue Cross Complete considers orthognathic surgery medically necessary for correction of skeletal deformities of the maxilla or mandible when clinical.