Independence Blue Cross offers products through its subsidiaries Independence Hospital Indemnity Plan Keystone Health Plan East and QCC Insurance Company independent. And each Blue Cross andor Blue Shield plan are independent licensees of the Blue Cross and Blue Shield Association.
 Understanding Medicare Before You Age In Blue Cross Mn
Understanding Medicare Before You Age In Blue Cross Mn
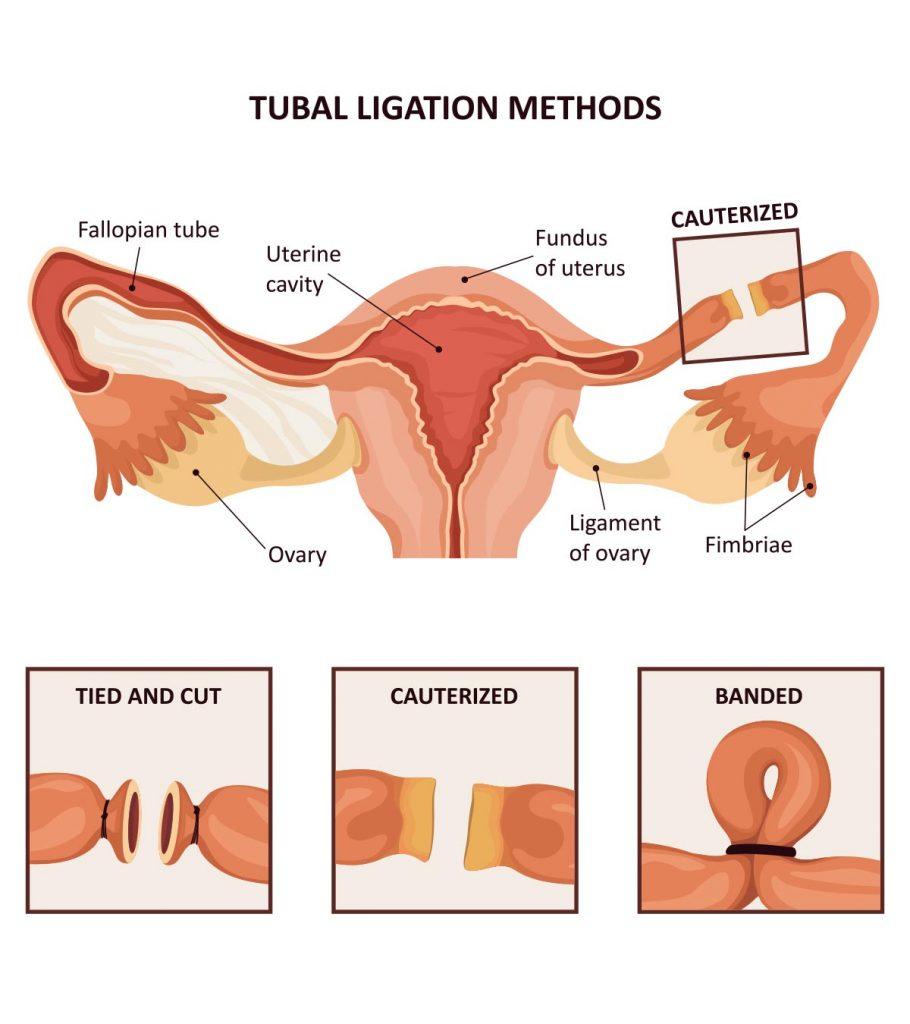
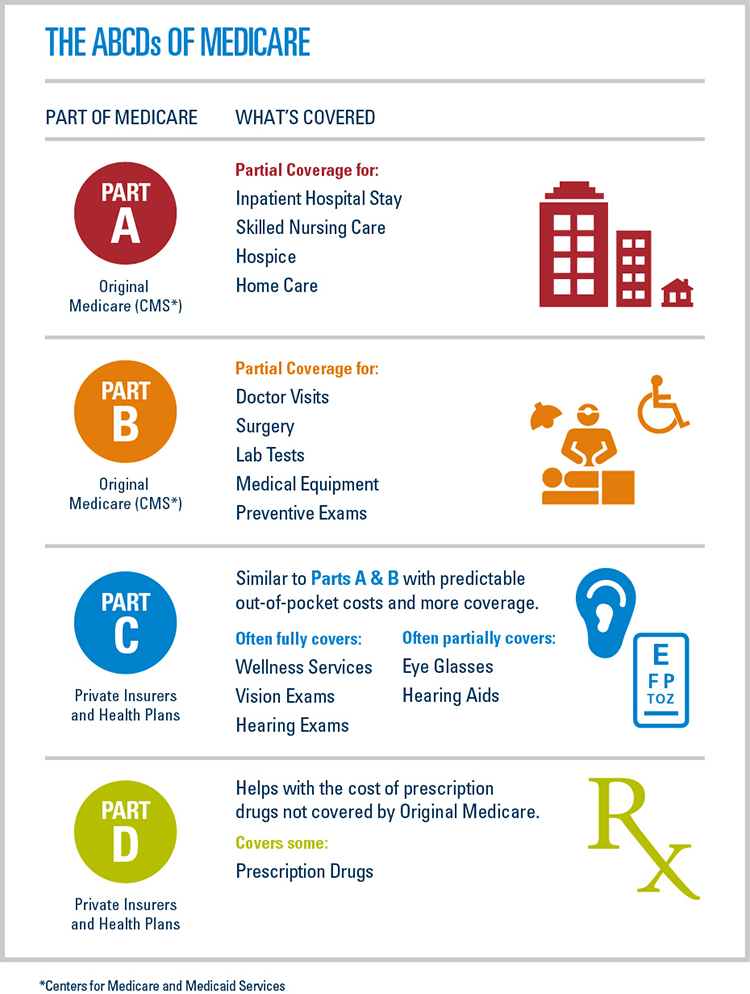
Medicare Part A hospital insurance covers inpatient hospital care skilled nursing facility hospice lab tests surgery home health care.
Basic medicare blue. Basic Plan K L N and F are Medicare Supplement plans without a network. Advertentie Shop 2020 Medicare plans. Enrollment in Basic Blue Rx depends on contract renewal.
Coordination of benefits with Blue. They combine all the benefits of Medicare Part A and Part B and usually include prescription drug coverage Part D. Enrollment in Independence Medicare Advantage plans depends on contract renewal.
Its priced as follows. Medicare Advantage MA plans are health plans offered by private organizations like Florida Blue that contract with Medicare. Made in the USA.
Basic Medicare Blue. Unique Formula With Real Ingredients. Many plans include additional benefits like dental hearing and vision.
Advertentie Over 174000 Trusted Users of Meticore. Is the underwriter for Basic Blue Rx PDP a prescription drug plan with a Medicare contract. Extended Basic Blue costs a little more but this plan has an out-of-pocket maximum and extended skilled nursing facility days.
Whether you are new to Medicare or want a refresher here are a few resources to help you understand the costs benefits and choices offered by Blue. Find out how Medicare works and what it covers and compare the 2 main ways to get your Medicare coverage. It might be different than you think.
Independence Blue Cross offers Medicare Advantage plans with a Medicare contract. Discover how all the parts of Medicare - A B C and D work. This is VERYimportant to ensure you get the most out of your coverage.
SilverSneakers is a registered trademark of Tivity Health Inc an independent company that provides health and fitness programs. When you select all four additional coverage options to a Basic plan youll have minimal out-of-pocket costs for Medicare-covered services. For more information about Medicare including a complete listing of plans available in your service area please contact the Medicare program at 1-800-MEDICARE TTY users should call 1-877-486-2048 or visit wwwmedicaregov.
Both Standard and Basic Option cover Preferred and Non-preferred drugs while FEP Blue Focus only covers Preferred drugs. Before you get into the details its important to understand some basic information about Medicare and how it can help you cover the costs of your health care. Enrollment in these Blue Cross plans depends on contract renewal.
Over the years it has changed. Medicare was established in 1965 to help people who are 65 and over or have disabilities pay for the rising costs of medical care. Blue Cross Medicare Advantage Platinum Blue Senior Gold and other Medicare Supplement and SecureBlue plans are eligible.
Your Medicare coverage choices. With the Blue Cross MedicareRx Basic PDP you have several different costs including the premium monthly a deductible annual and pharmacy co-pays andor co-insurance. Plans with prescription drug benefits have a pharmacy network.
For more information about Medicare including a complete listing of plans available in your service area please contact the Medicare program at 1-800-MEDICARE TTY users should call 1-877-486-2048 or visit wwwmedicaregov. Advertentie Over 174000 Trusted Users of Meticore. Find your best rate from over 4700 Medicare plans nationwide.
When its time to visit a doctor or hospital its important to choose one that is part of your Blue Cross Medicare plan network. MII Life Insurance Inc. A provider network is made up of all the doctors and hospitals that participate in your plan.
Each Blue Cross Blue Shield company is responsible for the information that it provides. Learn about the 2 main ways to get your Medicare coverage Original Medicare or a Medicare Advantage Plan Part C. Plans with combined medical and prescription drug coverage.
Find your best rate from over 4700 Medicare plans nationwide. About Press Copyright Contact us Creators Advertise Developers Terms Privacy Policy Safety How YouTube works. What Part B covers.
Blue Cross Medicare Advantage PPO Blue Cross Medicare Advantage MA Only PPO Blue Cross Strive Medicare Advantage HMO-POS Medicare Advantage Health Maintenance Organization Special Needs Plan HMO-SNP Description Senior Gold is a Medicare Select Supplement plan with a network. Advertentie Shop 2020 Medicare plans. Protect the best years ahead.
Made in the USA. Each Blue Cross Blue Shield company is responsible for the information that it provides. This plans annual premium is 73680 6140 paid monthly.
If you currently take prescription drugs you should check our approved drug lists formularies to ensure your drug is covered under your selected plan. MII Life Insurance Inc. Unique Formula With Real Ingredients.
What Part A covers. Protect the best years ahead.