For prior authorizations for services that were completed before Oct. Provider may complete a Face-To-Face assessment via telehealth.
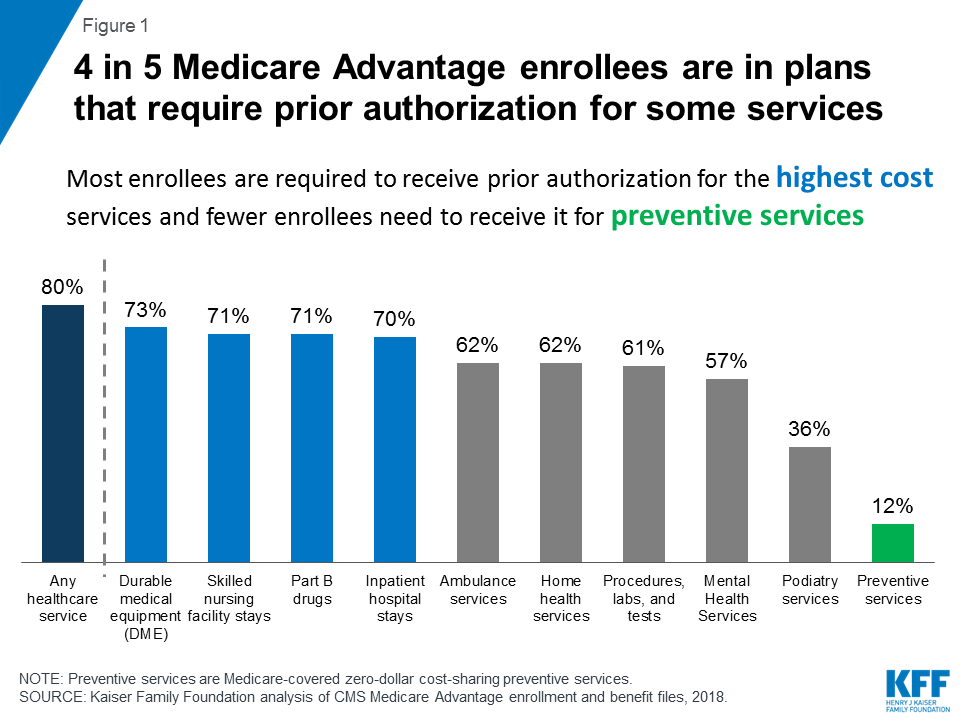 Prior Authorization In Medicare Advantage Plans How Often Is It Used Kff
Prior Authorization In Medicare Advantage Plans How Often Is It Used Kff
One-third of practices employ staffers who spend every second of.

How long does prior authorization take. Health insurance companies use the prior authorization or pre-approval process to verify that a certain drug procedure or service is medically necessary BEFORE it is done or the prescription is filled. Joe should allow his doctors office and insurance company enough time to complete their end of. Typically within 5-10 business days of hearing from your doctor your health insurance company will either approve or deny the prior authorization request.
Its especially important for insurers to be able to process prior authorization requests on weekends and after normal business hours during the week. Who decides what drugs to include in my Prior Authorization program. Your airline will refuse to allow you to board your flight.
Medical practices spend an average of two business days a week per physician to comply with health plans inefficient and overused prior-authorization PA protocols. There are a few lessons to take. Only your physician can provide this information and request a prior authorization.
What if I dont obtain the TCI Assured authorization. Sometimes an insurance company may want the patient to fill out some paperwork or sign some forms. At the high end 23 percent of respondents said they and their staff completed more than 40 prior-authorization requests in the week before taking the survey.
Information should be uploaded 24 hours prior to travel however shorter times can be accommodated. Authorization takes between 15 minutes and 24 hours. How long does this take.
If the request for prior authorization isnt approved your insurer will let you and your doctor know. A standard request may take up to 15 days for us to make a decision. If its rejected you or your doctor can ask for a review of the decision.
In 2009 one study estimated that on average prior authorization requests consumed about 20 hours a week per medical practice. 1 2019 or later UnitedHealthcare is extending prior authorizations through Sept. If the application is incomplete it may take longer.
For prior authorizations for services that were completed on Oct. How long does it take to get prior authorization. For example when dermatologists tracked how long it took patients at their practice to get a reply for prior authorization for a biologic medication they found that about half of their.
1 2019 a new prior authorization is required. One hour of the doctors time nearly six hours of clerical time plus 13 hours of nurses time. Pharmacist tells you that your prescription needs a prior authorization it simply means that more information is needed to see if your plan covers the drug.
What kinds of drugs need prior authorization. For an urgent review of a non-covered drug one not on your drug list we will have a decision in 24 hours or less. Insurance providers typically reply to a request for prior authorization within 30 business days and many providers could reply sooner.
How does prior authorization work. Physicians in the AMA survey said that turnaround varies from one business day to five or more. If that institution can delay handing back your pre-auth for a few more days it can use those funds for another purpose and thats what it does.
Twenty-three percent reported they and their staff completed between 21 and 40 PA requests while only 14 percent reported completing five or fewer. This is extremely important to know especially for people being treated for cancer. If you file an urgent request we will have a decision provided in 72 hours or less.
Your doctor will submit a prior authorization request before ordering a test or medication.