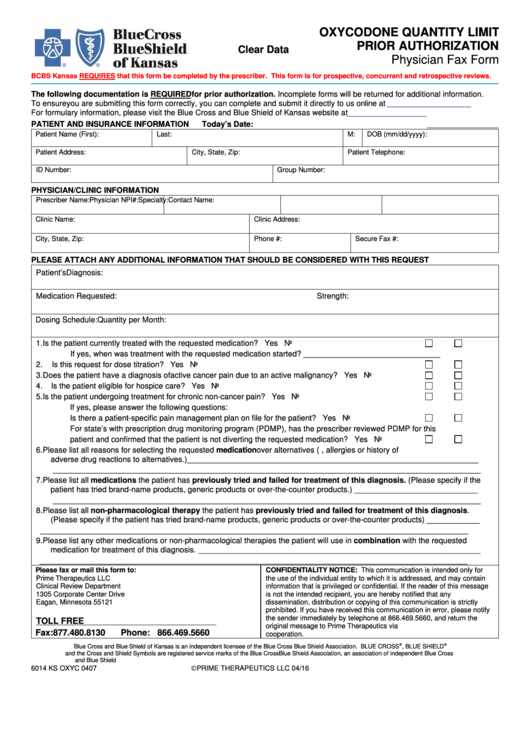
Incomplete forms or forms without the chart notes will be returned. Drug Prior Authorization Request Form Incomplete Form May Delay Processing An independent licensee of the Blue Cross and Blue Shield Association.
 Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
Top 28 Blue Cross Blue Shield Prior Authorization Form Templates Free To Download In Pdf Format
The form contains important information regarding the patients medical history and requested medication which Anthem will use to determine whether or not the prescription is included in the patients health care plan.
Blue shield prior authorization form. Forms and additional information can be downloaded on the CVS Caremark website. Box 411878 Kansas City MO 64141-1878. Open or download the list.
Usually the provider is responsible for requesting prior authorization before performing a service if the member is seeing an in-network provider. For some services listed in our medical policies we require prior authorization. Call 866-325-1794 to check the status of a request.
Page 2 of 2 Revised 122016 PRESCRIPTION DRUG PRIOR AUTHORIZATION OR STEP THERAPY EXCEPTION REQUEST FORM Patient Name. Weve provided the following resources to help you understand Anthems prior authorization process and obtain authorization for your patients when its required. This is a library of the forms most frequently used by health care professionals.
For questions related to medical authorizations find the appropriate phone number on Authorization contacts page. Search for the document you need to. Medications that Require Prior Authorization M indicates the pre-authorization is only required for Medex and Blue Care 65 members.
Blue Cross and Blue Shield of Minnesota and Blue Plus are nonprofit independent licensees of the Blue Cross and Blue. To find a prior authorization form visit our forms. This list shows prescription medications that require your doctor to obtain authorization from us.
To obtain a fax form go to the prior authorization forms page. Sometimes a plan may require the member to request prior authorization for services. If this information is not submitted or does not meet the prior.
Thank You for Being a Caregiver. Requests for the following services can be made by fax or mail. Prior Authorization Requirements for City of New York Employees Federal Employee Program FEP Precertification Requirements Use this list to identify the inpatient and outpatient services that require prior approval under FEP Standard Basic andor Blue Focus plans.
For questions related to pharmacy authorizations contact Pharmacy Services at 800 697-8122. A prior authorization is an approval review that Blue Shield of California Promise Health Plan conducts. Operated on behalf of the Blue Cross and Blue Shield Service Benefit Plan by a third party.
All requested data must be provided. Prior authorization forms for Blue Shield members Download and print prior authorization forms for procedures and drugs. Mail-in Requests for ACA and Medicare Advantage Plan Members Central Operations COPS Blue KC MA ACA PO.
You can download the Physician Request for Prior Authorization form also called the Formulary Exception form. Submit a prior authorization Reviewed by BlueCross BlueShield. Fax Requests for ACA and Medicare Advantage Plan Members 877-549-1744.
Medical Technology Assessment Non-Covered Services List 400. Prior Authorization Health insurance can be complicatedespecially when it comes to prior authorization also referred to as pre-approval pre-authorization and pre-certification. The protection of your privacy will be governed by the privacy.
Prior Authorization Mail Stop B5A1 PO. Blue Cross and Blue Shield of Kansas City Attention. Prescriber Information Patient Information Physician Name.
The Anthem Blue Cross Blue Shield prior authorization form is what physicians will use when requesting payment for a patients prescription cost. Contact Provider Services at 1-866-518-8448 for forms that are not listed. To request prior authorization for treatment or for a drug you your doctor other prescriber or appointed representative need to contact Blue Shield of California Promise Health Plan and provide necessary clinical information.
Medical and pharmacy authorization requests can also be faxed to Blue Shield. Get blue cross blue shield of alabama prior authorization form signed right from your smartphone using these six tips. Box 419169 Kansas City MO 64141.
If you dont have an account yet register. Information for Blue Cross and Blue Shield of Illinois BCBSIL members is found on our member site. Blue Cross Blue Shield of Massachusetts is an Independent Licensee of the Blue Cross and Blue.
Chart notes or lab data to support the prior authorization or step therapy exception request. Prior Authorization Quick Tips. Patient ID.
SM Marks of the Blue Cross and Blue Shield Association. Prior authorization list for Blue Shield including Medicare 65 and FEP members Search a list of medical services and procedures requiring prior authorization. Blue Cross and Blue Shields Federal Employee Program.
Please fill out all applicable sections on both pages completely and legiblyAttach any additional documentation that is important for the review eg.